Transverse fractures that involve the vertebrae, discs and ligaments are usually due to distraction mechanisms, associated with either flexion or extension. These are categorized as Type B fractures in the AOS system with three subtypes described: Transosseous tension band injuries (B1, Chance fractures), posterior tension band injuries with anterior compression (B2, flexion-distraction injuries), and hyperextension injuries (B3).
The Chance fracture (B1) is a pure transverse fracture, either through the vertebra, the disc, or both, with preservation of the anterior vertebral body height. The flexion distraction injury (B2) results from a combination of anterior compression (as in type A injuries), and transverse fracture due to posterior ligament failure. Historically seen in patients in motor vehicle accidents who were restrained by lap belts, these fractures are always unstable and require surgical fixation.
If CT is unavailable, AP and lateral radiographs can identify the horizontal fracture through the spinous process, laminae, or pedicles, distraction of the spinous processes, and any loss of anterior vertebral height. CT is preferred in suspected spinal fracture and thin-section axial images with coronal and sagittal reformations sensitively evaluate the extent of injury, any associated disk disruption, and degree of spinal canal compromise.


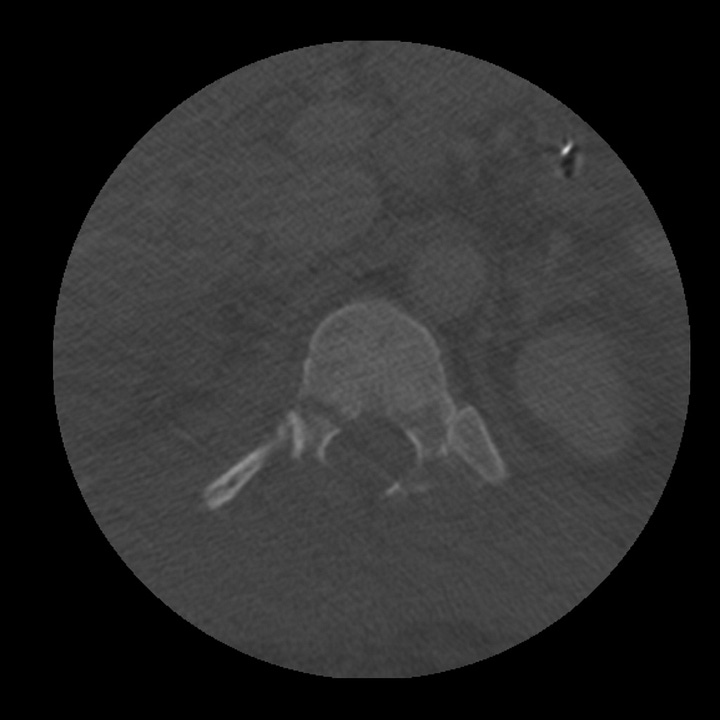

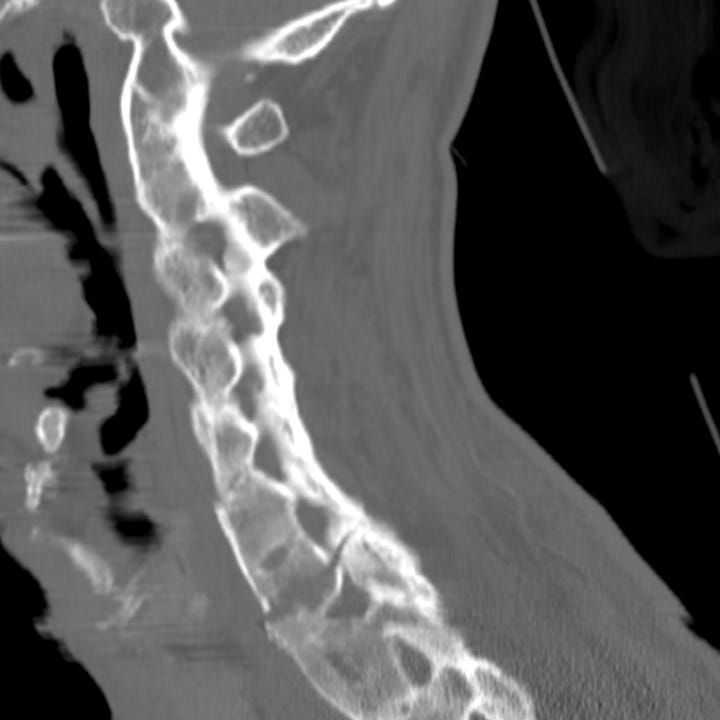
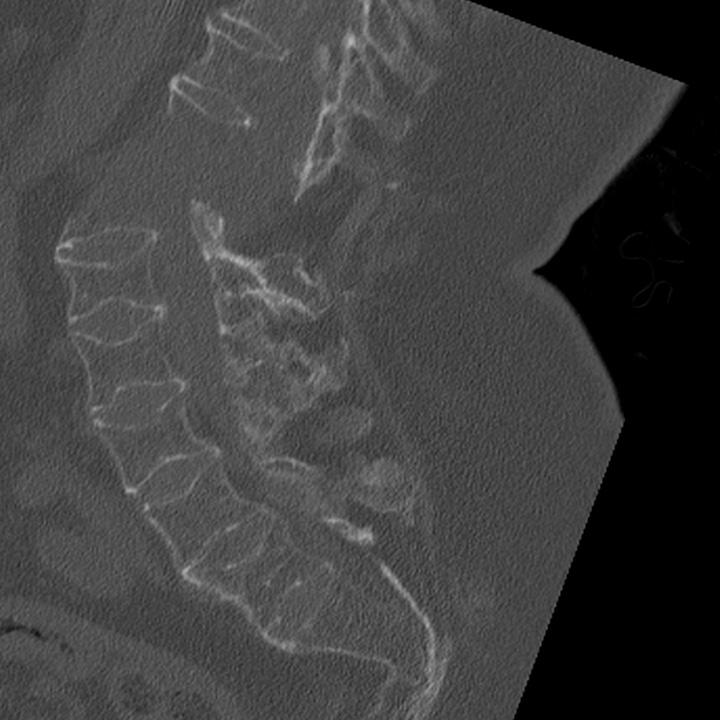
Chance fracture. T12 horizontal fracture through the vertebral body and pedicles. No vertebral body height loss. Associated hepatic laceration. Note increased interspinous distance on sagittal CT reformation and “disappearing” pedicle on axial image (case courtesy of Mark Bernstein, MD).
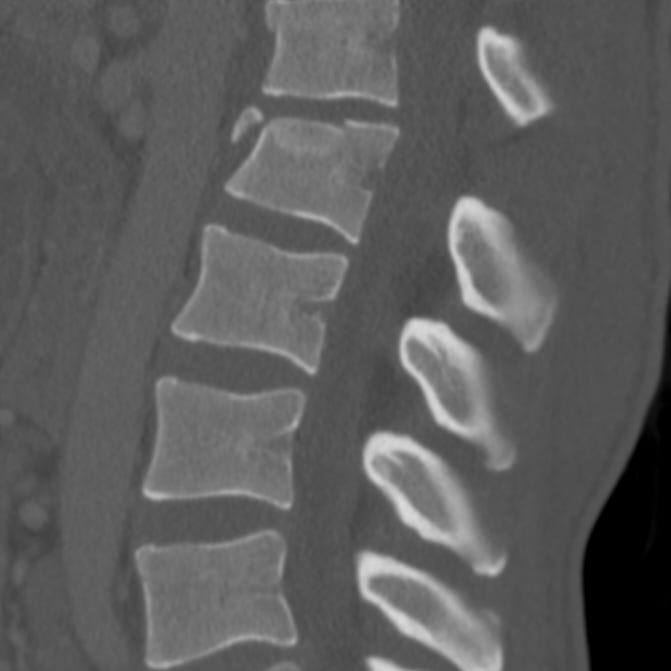


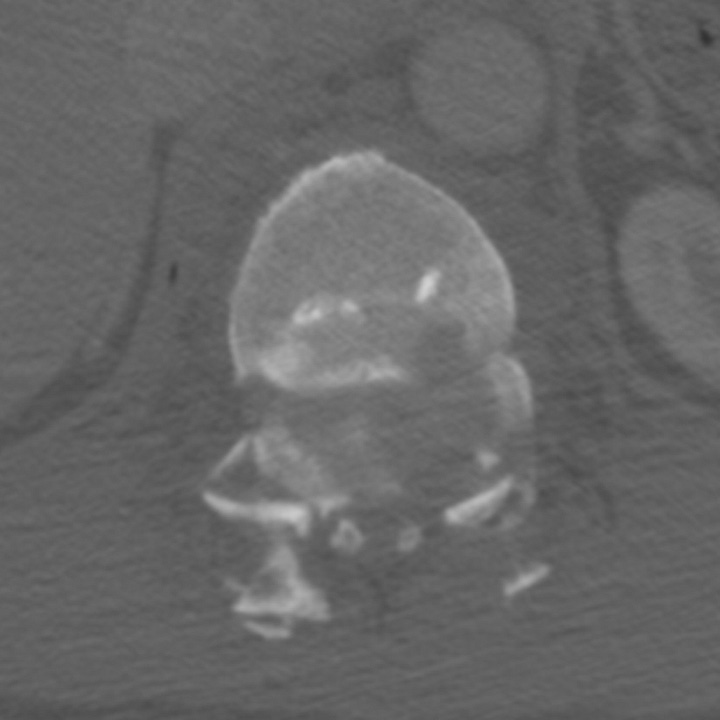
L1 flexion-distraction injury. L1 vertebral body fracture with anterior height loss and angulation, fractures through the anterior and middle third of the vertebral body, and distracted T12–L1 spinous processes. The inferior articulating facets of T12 do not articulate with the superior articulating facets of L1 on axial CT images (“naked facet”).


Flexion-distraction injury with spinous process fracture. Anterior L1 compression with horizontal fracture through the inferior articulating facets and spinous process of T12.
Flexion-distraction and Chance fractures are often associated with abdominal visceral injury, particularly proximal intestinal and pancreatic contusion. Abdomen and pelvis CT with intravenous contrast should be always be obtained in this setting
Hyperextension injuries (B3) are most commonly seen in patients with fused spines. Altered biomechanics in patients with ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, osteogenesis imperfecta, and ossification of the posterior longitudinal ligament, results in a rigid, brittle spine that is vulnerable to both hyperextension and hyperflexion injuries. In hyperextension injuries the anterior longitudinal ligament is disrupted, with variable involvement of posterior elements. If intact, the posterior ligaments may prevent complete dislocation. The entire spine should be imaged in all patients with fused spines, as multiple fractures are often present.
Lateral spine radiographs or CT with sagittal reformation show a horizontal or oblique fracture, often through all spinal columns. Dislocation may not be obvious, particularly after immobilization, and failure to identify a fused-spine fracture in the neurologically intact patient can result in delayed neurologic decompensation.
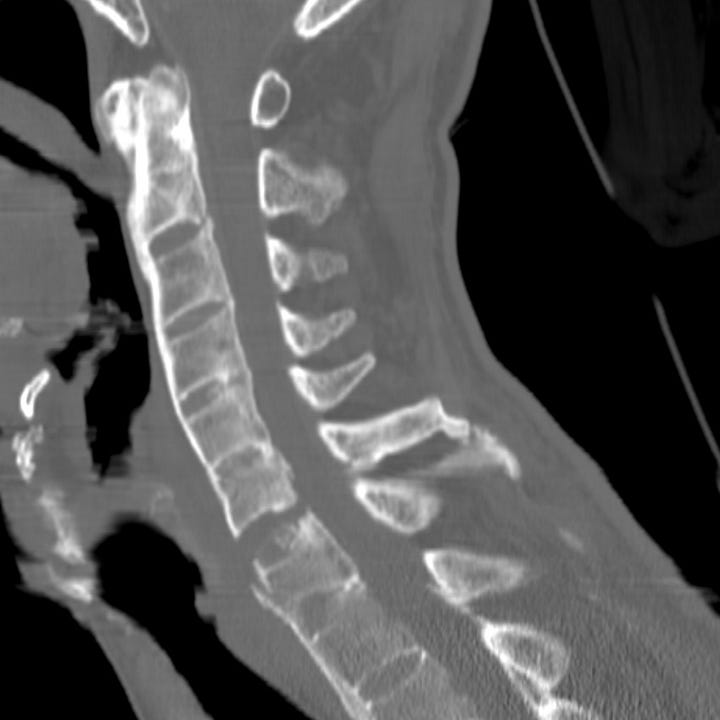
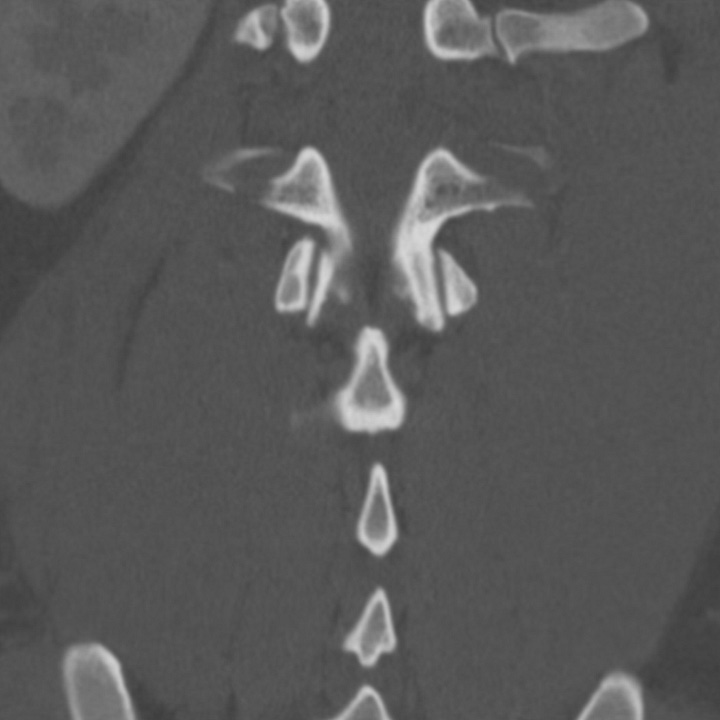
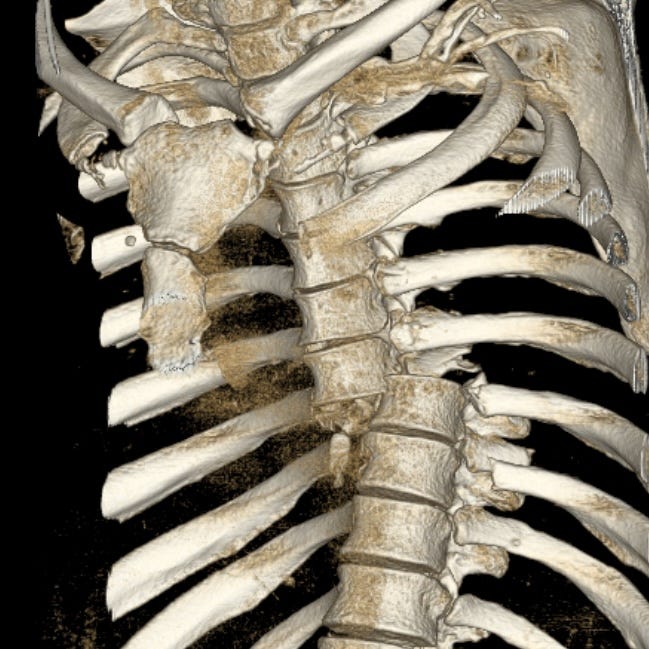
Fused-spine fracture in ankylosing spondylitis. Fracture through fused C6 and C7 vertebrae.

Fused-spine fracture-dislocation in osteogenesis imperfecta. Fracture through the T12 vertebra with marked distraction and displacement.


Hyperextension fracture-dislocation in a patient with diffuse idiopathic skeletal hyperostosis (DISH). Displaced upper thoracic horizontal fracture through partially involving the intervertebral disc with associated paraspinous hematoma, pulmonary contusion, and rib fractures.
Spinal fracture-dislocation (AOS type C) is the most severe type of thoracolumbar fracture and is a grossly unstable injury, characterized by disruption of all three spinal columns and complete neurologic deficit below the affected level. It is due to severe, complex, shearing and rotational forces most commonly seen in motor vehicle collisions, impact from heavy objects, or falls. Surgical immobilization is almost always necessary to permit spinal stabilization and rehabilitation. Neurological deficits are usually immediate and permanent.
Fracture-dislocations can be detected on the initial supine AP radiograph obtained during resuscitation, and spinal continuity should always be carefully assessed. Most patients with an injury mechanism powerful enough to cause a spinal dislocation will undergo chest and abdominal CT, which better characterizes fracture-dislocations and detects any associated visceral injury. Translation or rotation of the spine above and below the level of injury is diagnostic and best appreciated on sagittal, coronal, or 3D reformations. Axial findings include non-articulating (“naked”) facets and visualization of two adjacent vertebrae on the same axial image (“double vertebra”).

Fracture-dislocation with anterior translation. T11 is anteriorly sublimed with respect to T12. Anterior T12 wedge deformity and wide splaying of the spinous processes indicate failure of anterior, middle, and posterior columns. The T11 and T12 vertebrae are both visible on the same axial image.



Fracture-dislocation with anterior and transverse translation and rotation. CT scout image shows discontinuity of the mid-thoracic spine. The T7–T8 intervertebral disk space is completely disrupted, with anterior and transverse dislocation of T7 with respect to T8, large paraspinous hematoma, soft tissue gas,posterior pulmonary contusions, and a right pleural effusion/hematoma.
Further reading and reference
AO Spine Thoracolumbar Injury Classification System
Thoracolumbar Spine Fracture (National Library of Medicine - StatPearls)



