Vertebral osteomyelitis/discitis is a bacterial or mycobacterial infection of the disc and adjacent vertebrae frequently associated with paraspinal or epidural abscess. Because of its rich blood supply, especially in children, hematogenous infection usually begins at the intervertebral disc and subsequently extends to the adjacent vertebrae and epidural space. In older adults, vertebral osteomyelitis may result from a contiguous soft tissue infection or direct inoculation in trauma or as a surgical complication. Staphylococcus aureus is the most commonly encountered pathogen, but Streptococcus viridans is more characteristic of infections in intravenous drug users and immunocompromised patients. Immunosuppression due to diabetes is the most common risk factor. Others include:
HIV
Malignancy
Alcohol use
Hepatic or renal failure
Rheumatoid arthritis
Other immunosuppressive conditions
Indwelling catheter
Intravenous drug use
Recent spinal surgery
Infection elsewhere in the body
Patients typically present with insidious onset of focal neck and/or back pain, sometimes associated with systemic symptoms, fever, or neurological deficit.
The characteristic imaging finding is destruction, sclerosis, or edema that involves two adjacent vertebral bodies with loss of the interposed disk. Vertebral metastatic disease typically does not involve the disc. Tuberculous osteomyelitis often spreads between adjacent involved vertebrae via the paraspinous soft tissues or epidural space and can, but does not necessarily, spare the disc.
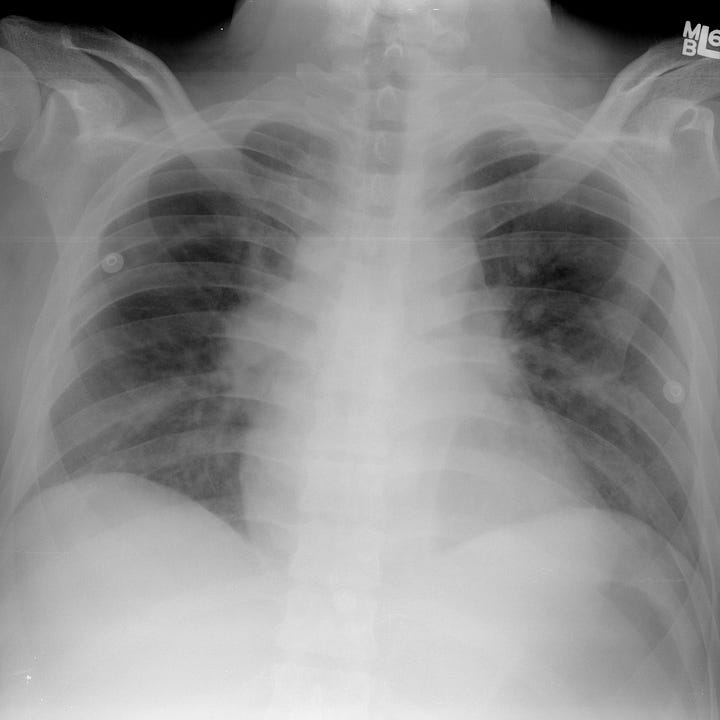

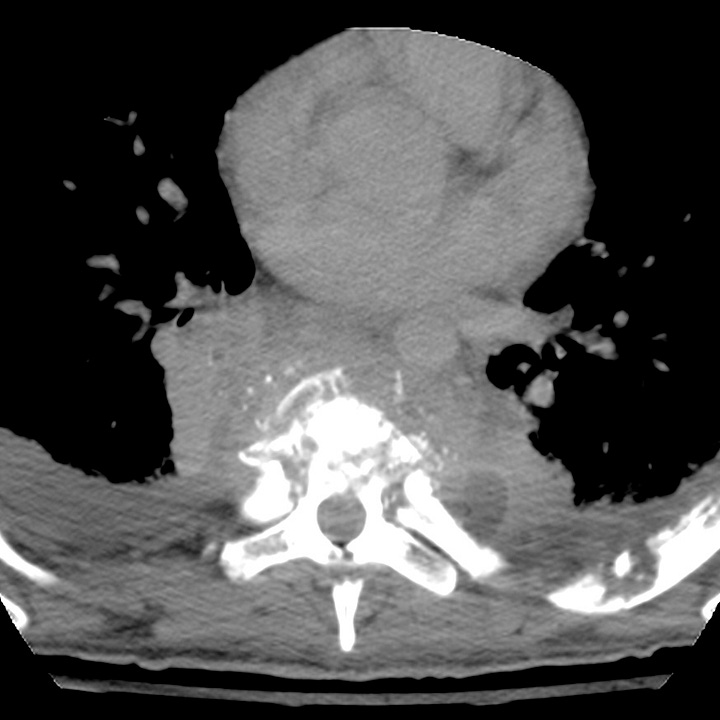

Bacterial discitis osteomyelitis. Frontal chest radiograph demonstrates widened paraspinous soft tissues and subtle hilar prominence. CT with coronal and sagittal reconstructions shows a large paraspinous soft tissue mass, obliteration of the T6 and T7 intervertebral disk spaces, T5 through T7 vertebral sclerosis, and end plate irregularity/erosion at T5–T6 and T7–T8. Bilateral pleural effusions, left sided rib destruction and a small left paraspinous abscess are evident. Focal mid-thoracic kyphosis is due to T5, T6, and T7 anterior collapse.
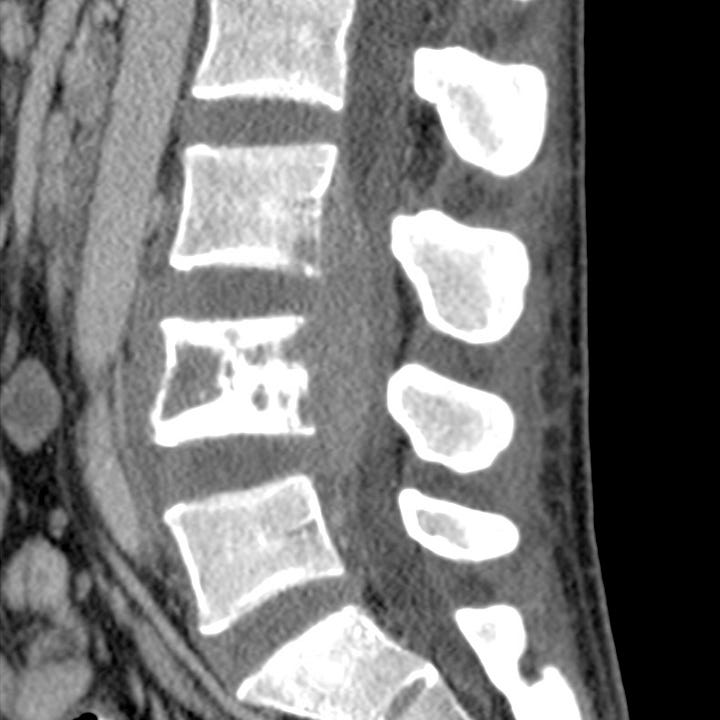

Tuberculous osteomyelitis. Sagittal CT reformation and T1 postgadolinium MRI show L4 sclerosis and areas of vertebral destruction with bridging prevertebral and epidural soft tissue masses. Subtle edema and erosion is evident at the posterior/inferior L3 endplate. The L3–L4 and L4–L5 intervertebral discs are normal.
Plain radiographs are usually the first study obtained for nonspecific back pain. They are insensitive to early discitis and may not indicate any abnormality for up to 4 weeks. Patients with risk factors should be imaged with MRI (preferably) or CT.
MRI with intravenous contrast is the most sensitive modality and should be the first study obtained if available. CT with contrast or CT myelography are alternatives. T2-weighted images show increased signal in the disk and adjacent vertebral marrow. Other potential findings on both T1- and T2-weighted sequences include vertebral collapse, vertebral body endplate destruction, paraspinous soft tissue/fluid collections and epidural abscess.
CT findings can be subtle in early disease and may only show mild loss of disk height and subtle endplate irregularity indistinguishable from degenerative change. Vertebral collapse, paraspinal or epidural inflammation, and abnormal paravertebral soft tissue or peripherally enhancing fluid collections indicate advanced or progressive disease.
Blood cultures usually reveal a causative agent, but if they are negative and imaging findings point to osteomyeltis/discitis, image guided biopsy or fluid aspiration is necessary. Medical therapy consists of long-term antibiotic treatment. Surgery may be indicated for cord compression or debridement in the case of antibiotic therapy failure



