Traumatic intrapleural hemorrhage is most commonly due to intercostal or internal mammary artery disruption and may be seen in either blunt or penetrating injury. Hemothorax due to pulmonary parenchymal injury from stabbing or contusion is often small and self-limited because of the low pulmonary vascular pressure and usually subsides spontaneously or following placement of a pleural drain.
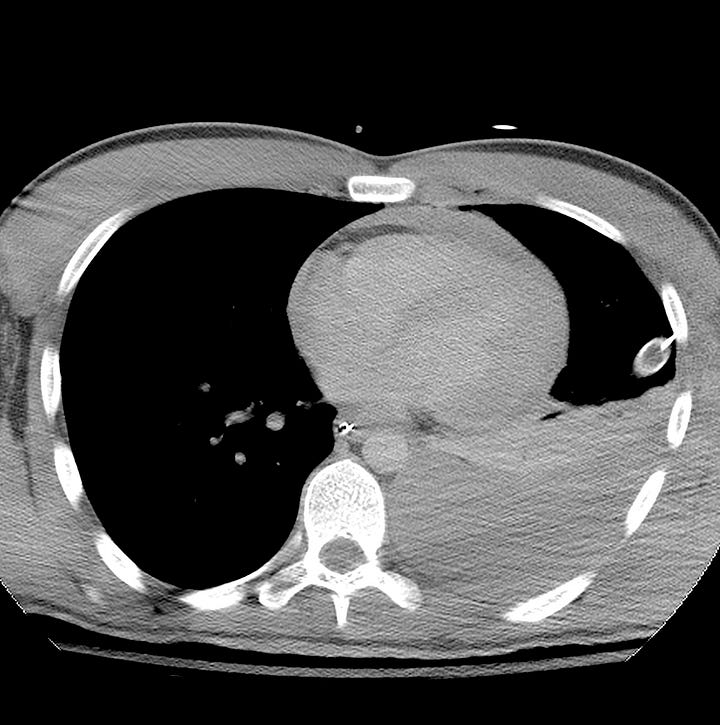
Massive hemothorax (> 1 liter) is due to arterial or large venous injury and presents with clinical signs of shock and hypoperfusion. It is a surgical emergency due to potential heart and great vessel tamponade from the accumulated blood, acute hypovolemic shock, and hypoxia from lung collapse.
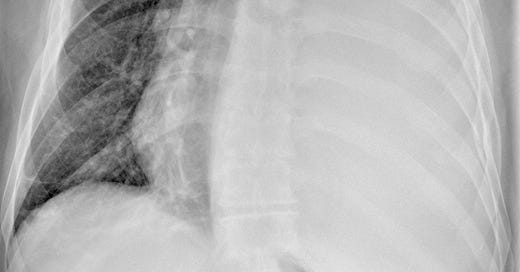
Hemothorax (stab wound). Massive left intrapleural fluid collection with compressed adjacent lung, contralateral mediastinal shift, and depression of the ipsilateral hemidiaphragm.
Supine chest radiographic findings are often subtle, depending on the volume of blood. Hazy increased density of the involved hemithorax with preserved vessel definition may be seen in smaller posterior hemothoraces. Large amounts of blood can fill the pleural space lateral to the lung and appear as a dense crescent-shaped collection.
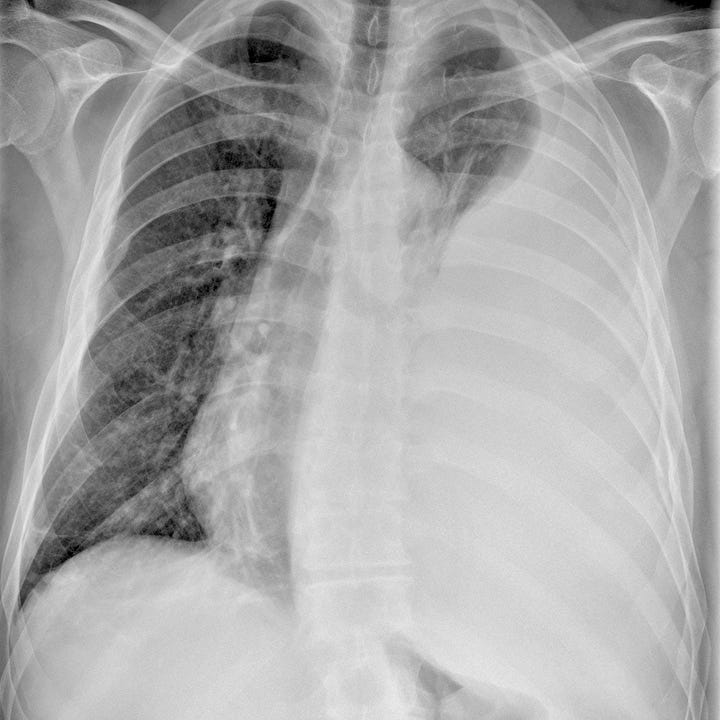
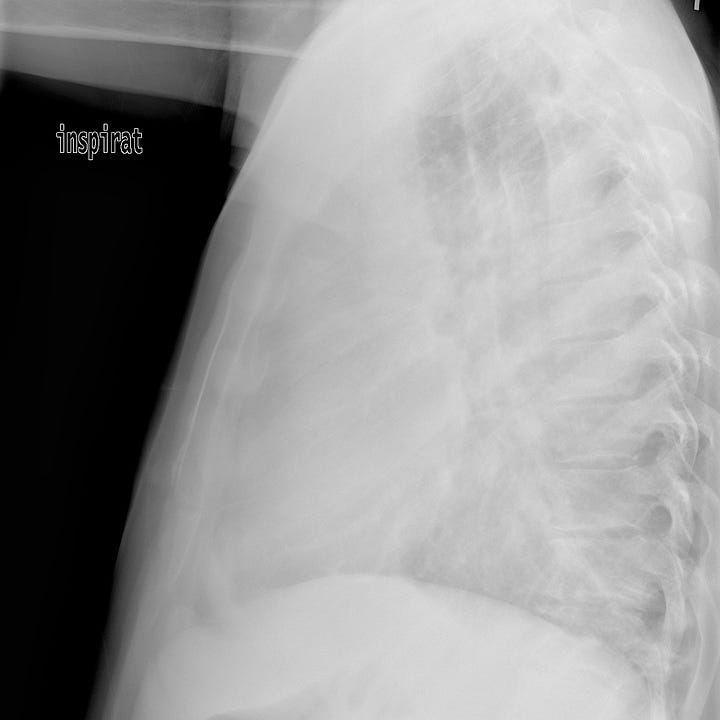
Hemothorax (stab wound). Supine radiograph with hazy opacification of the left hemithorax and preservation of the right heart border. CT shows large left posterior blood collection, with lower lobe compressive atelectasis.
CT with arterial-phase contrast enhancement is diagnostic; acute blood products have an attenuation of 35–70 HU, and layering of intrapleural fluid with different densities due to combinations of clot, blood cells, and serum can be seen. In addition, arterial phase CT evaluates the integrity of the great vessels, detects of any foci of arterial extravasation that may be amenable to embolotherapy, and identifies concomitant pneumothorax as well as any other visceral injuries.

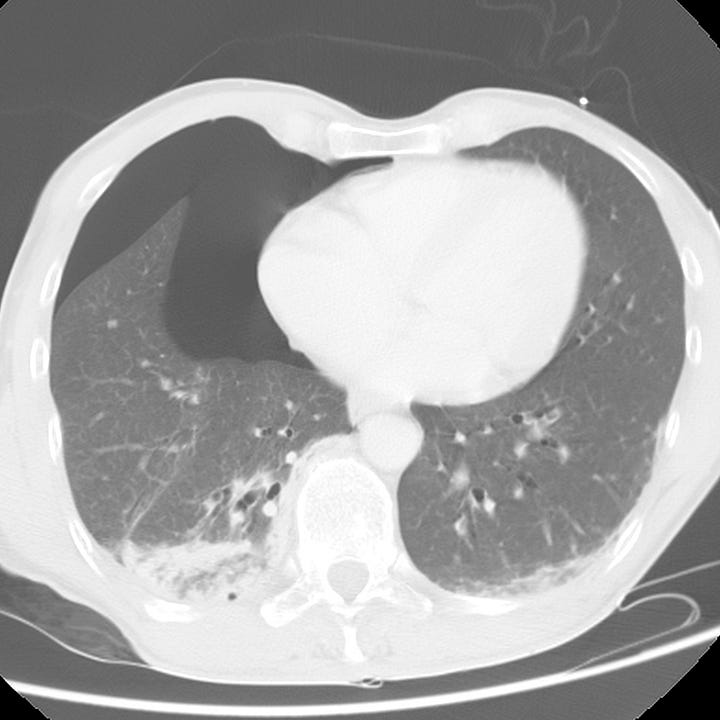
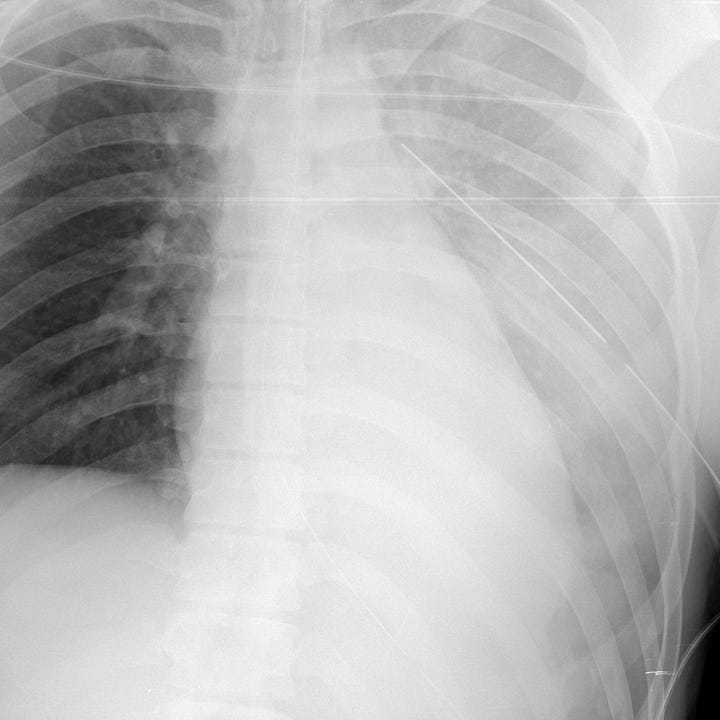
Hemopneumothorax (bicyclist struck by car). Moderate right pneumothorax, small hemothorax with lower lobe compressive atelectasis.
Initial management is by placement of a chest tube, which permits evacuation of clot, re-expansion of the collapsed lung, and effective tamponade of low-pressure bleeding. Definitive surgical management depends on the nature of the injury and source of hemorrhage.