Traumatic axonal injury, also known as diffuse axonal injury or shear injury, refers to cerebral neuronal damage that occurs when the brain is subjected to severe rotational and translational forces in trauma. Because gray and white matter densities are not identical, differential movement of the cortex relative to white matter during rapid acceleration shears traversing axons and perforating vessels. It is usually the consequence of high-velocity motor vehicle accidents or falls in which the patient typically suffers an immediate loss of consciousness and remains in a persistent vegetative state.
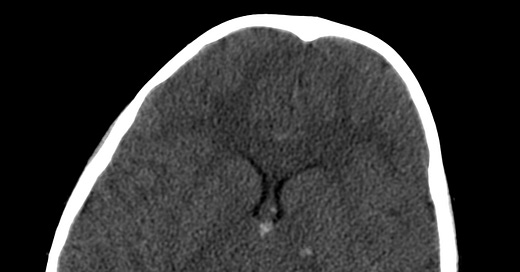
On CT imaging, small petechial hemorrhages from laceration of tiny perforating vessels indicate the presence of shearing neuronal injury. These are located at the gray-white junction of the cerebral hemispheres, the basal ganglia, the corpus callosum, or the dorsolateral midbrain. The depth of the hemorrhage roughly correlates with trauma severity. Generalized cerebral swelling and traumatic subarachnoid hemorrhage may also be seen..
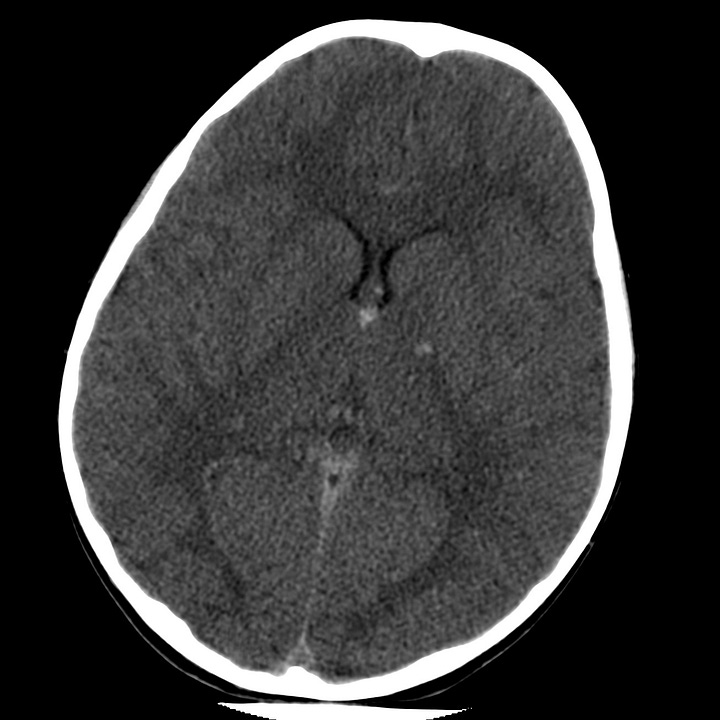
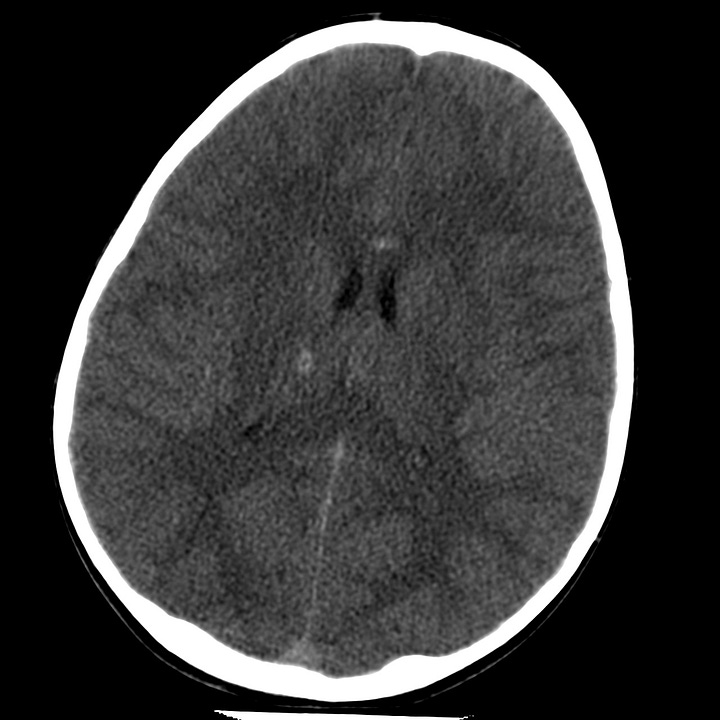
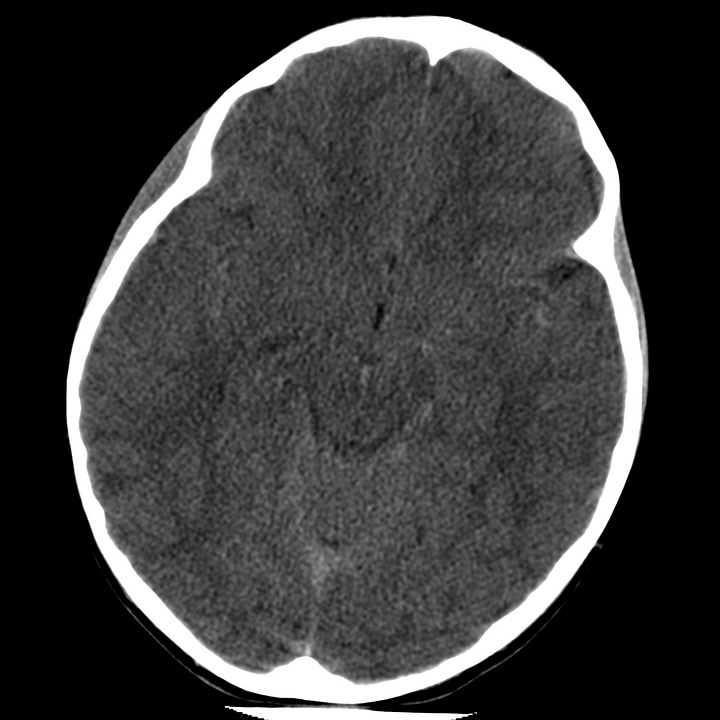
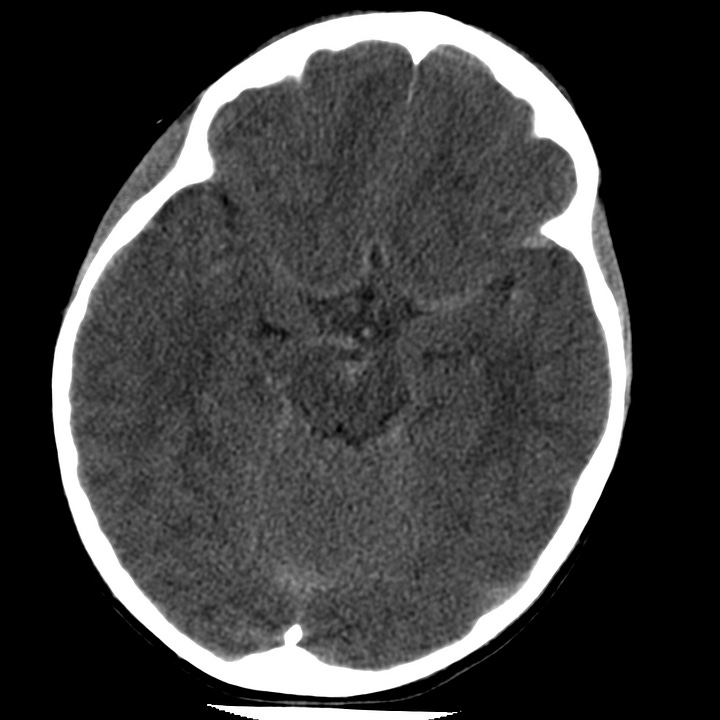
Traumatic axonal injury. Punctate hemorrhages at the gray-white matter junction involve the anterior corpus callosum, right thalamus, and left posterior limb of internal capsule. Associated traumatic subarachnoid hemorrhage is visible within the interpeduncular cistern and left quadrigeminal plate cistern.
CT can also appear completely normal, and while gradient-echo, and diffusion-weighted MRI is more sensitive for detection of micro-hemorrhages, both techniques are likely to underestimate the extent of axonal injury. In patients who survive significant head injury, later Wallerian degeneration of sheared axons, brain atrophy, and ventricular enlargement reveal neuronal damage that is often not apparent on initial CT.