Cerebrospinal fluid that leaks into the subdural space via either a tear or an irritation of the arachnoid membrane results in a subdural hygroma. Frequently bilateral, subdural hygromas are located over the anterior frontal or temporal lobes and usually become evident on CT 2 to 3 days after acute head trauma.

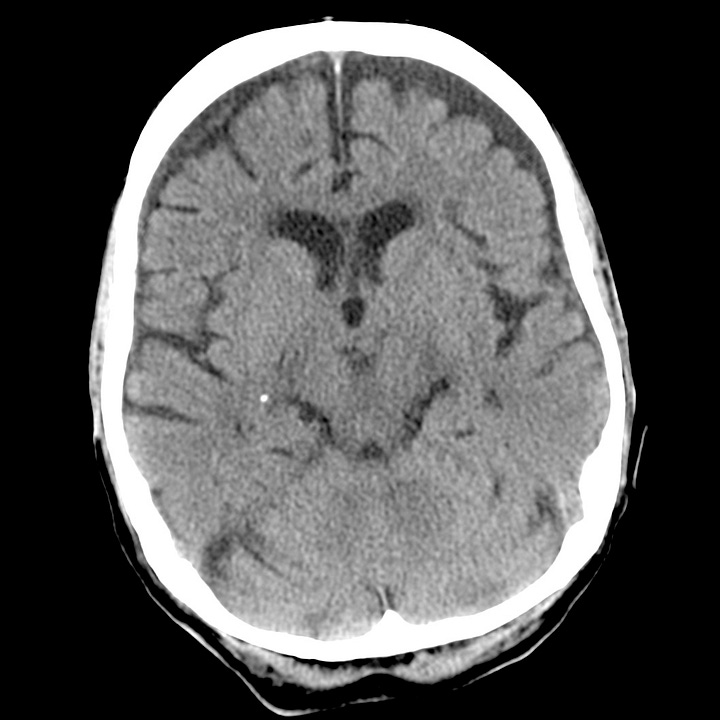
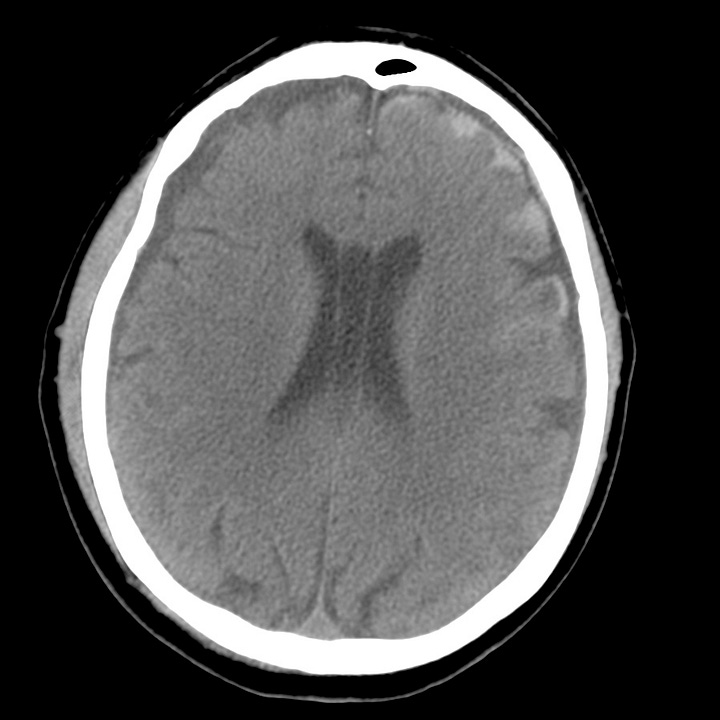
Subdural hygroma. The image at left, obtained at the time of injury, shows underlying ventricular and sulcal prominence. CT performed 48 hours later demonstrates interval appearance of symmetric, low-attenuation bifrontal subdural fluid collections.
Depending on CSF absorption and evolving post-traumatic brain swelling, subdural hygromas can fluctuate in size over time. Atrophy or encephalomalacia affords a potential space for the development of hygromas, whereas parenchymal expansion and fluid reabsorption will speed resolution of the hygroma.
Subdural hygromas have the same CT density as CSF and can be indistinguishable from chronic subdural hematomas. When isolated and identified in the setting of acute trauma, subdural hygromas are considered a benign consequence of head injury, since most are small and clinically insignificant, and do not require surgical intervention. Subdural hygromas are commonly seen in conjunction with other brain injuries, such as contusion, traumatic subarachnoid hemorrhage, and extra-axial hematomas.

Subdural hygroma associated with cortical contusion, epidural hematoma, and traumatic subarachnoid hemorrhage. Low-attenuation bifrontal subdural collections. High-attenuation traumatic subarachnoid hemorrhage fills the left frontal sulci. Left inferior frontal hemorrhagic contusion. Small right temporo-occipital epidural hematoma containing air.

