Subdural hematomas evolve over time. Hyperacute hemorhage, seen in the rare patient imaged immediately after injury, can be hypodense or mixed-density. Most patients are imaged after coagulation has taken place, and acute subdural hematomas are typically both hyperdense and crescentic. As an acute hematoma ages, protein degradation occurs, extracellular fluid shifts into the hematoma, and its density decreases.
Two to three weeks after injury, a subdural hematoma may be isodense to the adjacent cortex and difficult to detect, especially if small or bilateral. MRI or CT with contrast superior to non-enhanced CT for identification of these subtle hematomas. Subdural hematomas of any age can be complicated by rehemorrhage, which can convert a small, well-tolerated blood and serum collection into a larger, symptomatic mass.

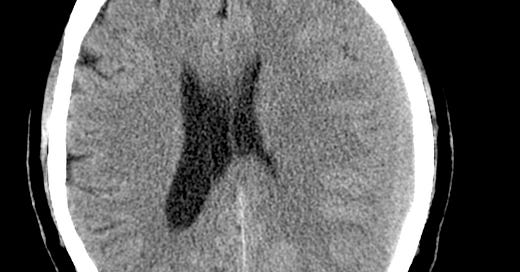
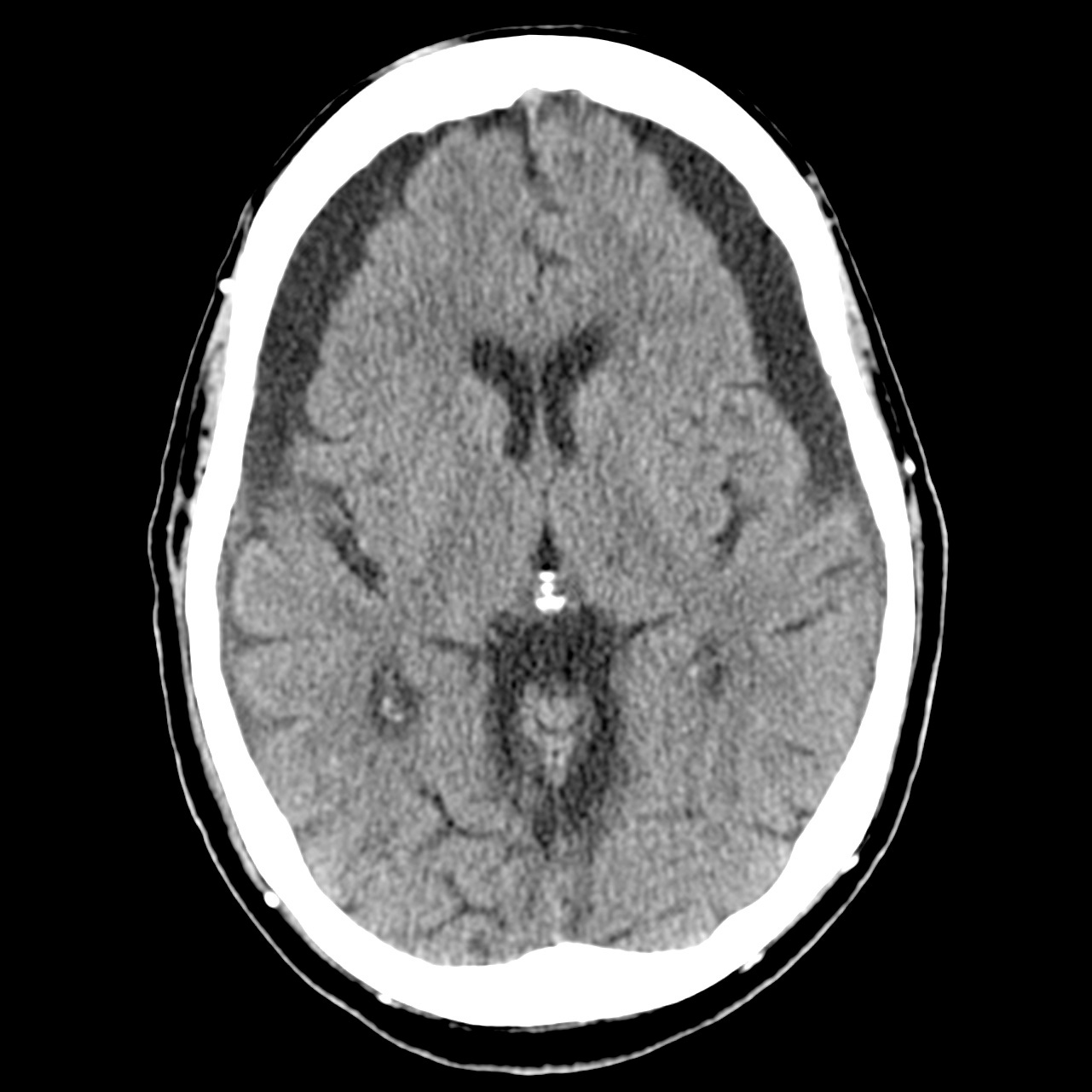
Subacute subdural hematoma. CT: left holohemispheric subdural hematoma, near isodense to cerebral cortex. Effaced left sulci and lateral ventricle with slight left to right subfalcine shift. MRI: T1-weighted image more clearly shows extent of subdural hematoma.
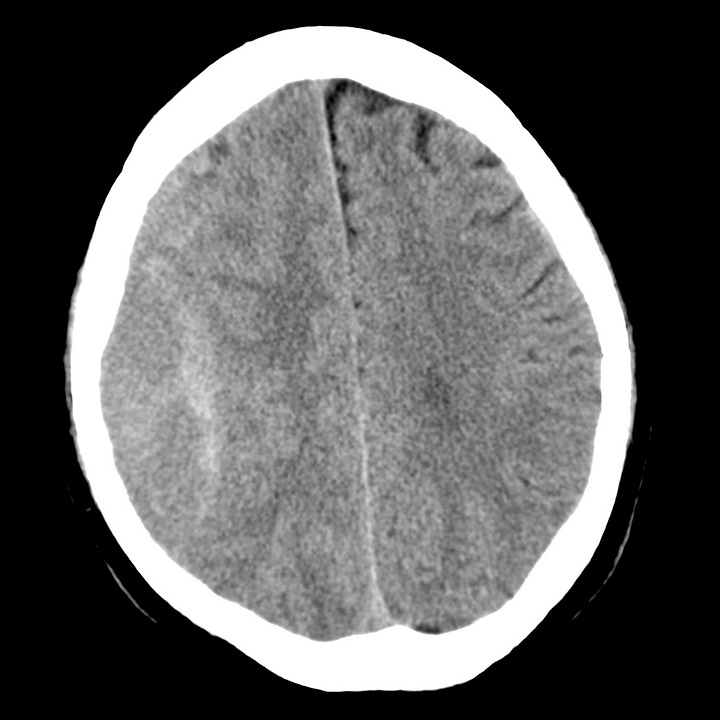
Three weeks or more after initial hemorrhage, a subdural hematoma is considered chronic. By this time, most simple hematomas are hypodense compared with brain and approach the density of cerebrospinal fluid, although they may contain areas of organized clot. Unevacuated hematomas incite a local inflammatory response that leads to formation of a fibrinous capsule and fragile, vascularized membranes. These can rupture spontaneously or with minor trauma, and patients who have had a previous subdural hematoma are at increased risk of subsequent hemorrhage.
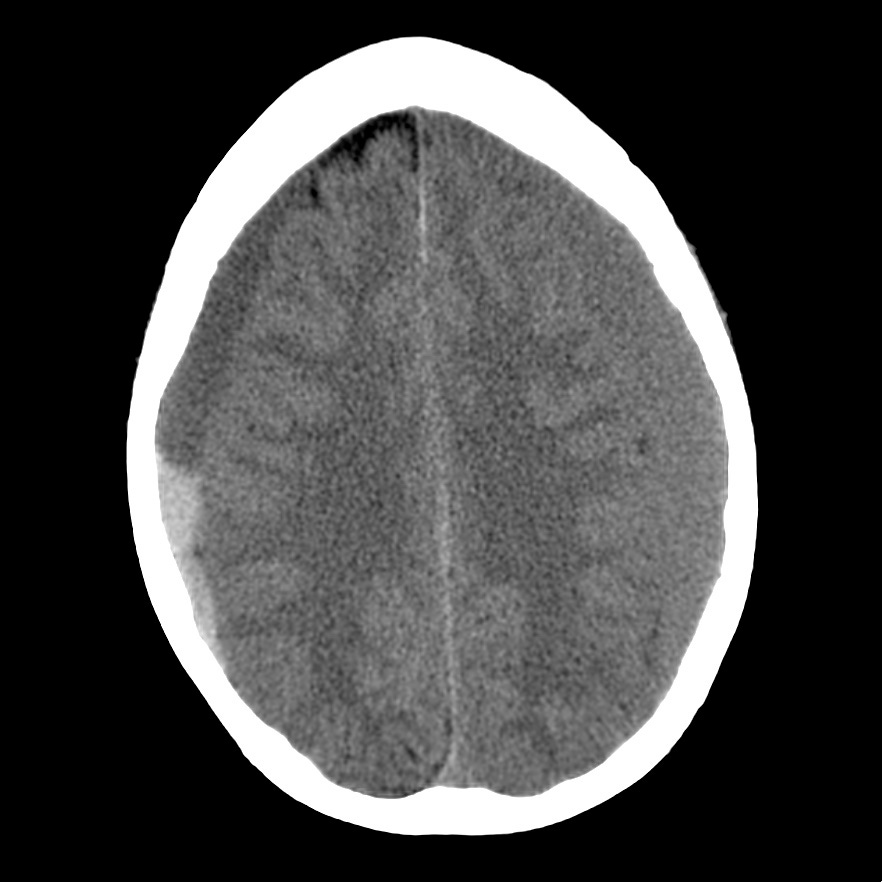
Chronic subdural hematoma. Low-attenuation subdural fluid collections with minimal dependent blood products. Underlying cerebral volume loss and moderate symmetric compression of the frontal brain parenchyma.
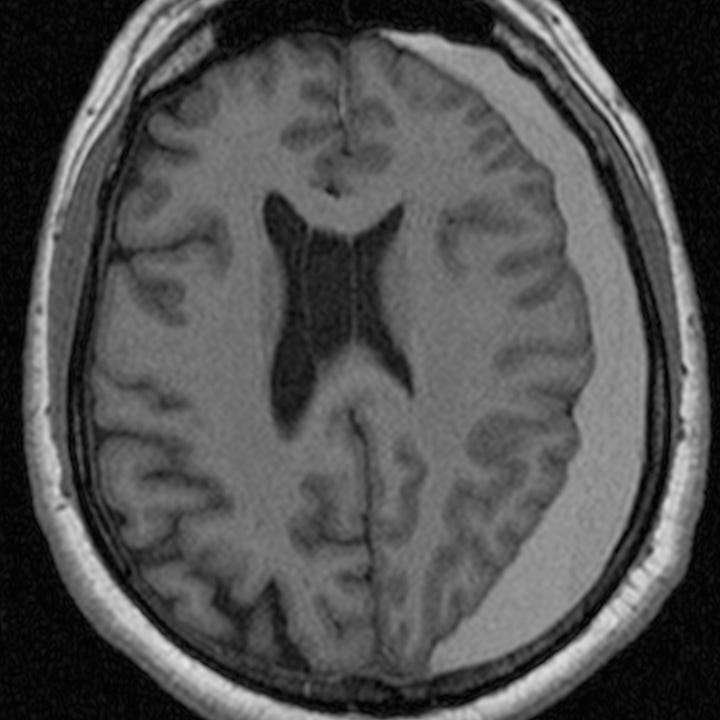
Delayed bleeding appears as hyperdense clot within the lower-density hematoma. Rehemorrhage into a chronic subdural hematoma may also appear convex rather than crescentic due to confinement by inflammatory membranes and can therefore mimic an epidural hematoma
.Chronic subdural hematoma with rehemorrhage. Left, isodense SDH. Right, low-density SDH with layering blood products.
Blood fluid levels are often seen in patients with chronic or subacute subdural hematomas after rehemorrhage. If a blood fluid level is seen in a patient with an acute or subacute subdural hematoma, it suggests an underlying hypocoagulable state or anticoagulant therapy.
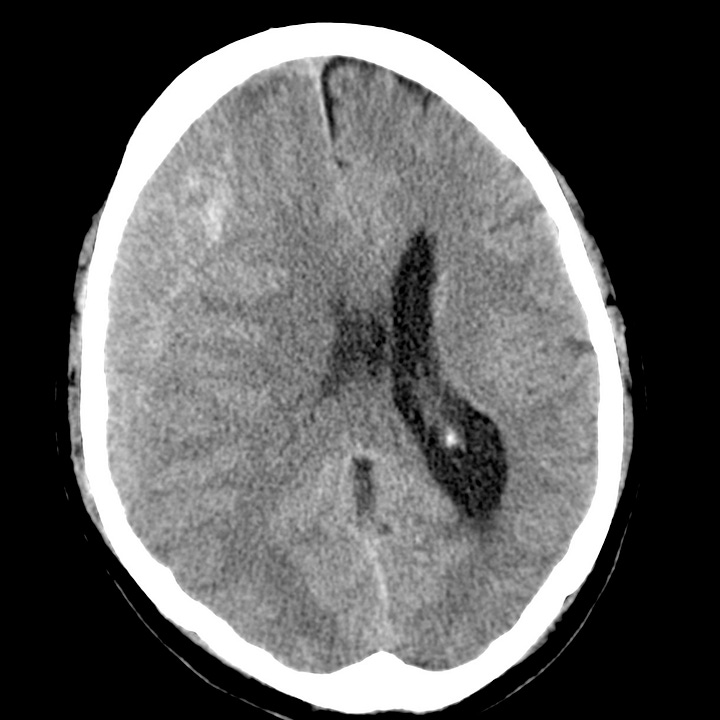
Complex subdural hematoma. Rehemorrhage with mixed density and lenticular shape due to con- finement of clot by membranes.
Chronic subdural hematoma can present with subtle or gradually progressing neurologic findings and no recalled history of trauma. Patients usually have underlying cerebral volume loss that can occur with advanced age, in chronic alcoholism and with remote head trauma. While the initial hemorrhage is asymptomatic, as the clot lyses and fluid enters the subdural space under osmotic pressure, an initially small collection can become large enough to result in neurologic deficit from cortical compression/ischemia or compartmental shift.