Splenic hematoma, laceration, devascularization, or frank rupture are potential consequences of blunt or penetrating injuries to the left torso. Patients may present with diffuse abdominal pain or left upper quadrant tenderness. Associated left shoulder pain is referred to as the Kehr sign. Leukocytosis and hyperamylasemia may also be seen. Hemodynamic stability, rather than grade of injury, directs initial management and surgical decision making.
During initial evaluation and resuscitation, FAST (Focused Assessment with Sonography in Trauma) quickly identifies intraperitoneal hemorrhage but is insensitive for visceral injury. Contrast-enhanced CT scan is the most accurate test for evaluating the spleen and should be obtained in the hemodynamically stable patient.
On CT, lacerations appear as nonenhancing linear or jagged lesions, often at the splenic periphery. They are associated with pericapsular or subcapsular hematomas, a crescent-shaped soft tissue attenuation fluid collection. This finding permits differentiation from splenic clefts, a normal variant. Splenic hematomas appear as low-attenuation intrasplenic masses.
Contrast extravasation on arterial phase images, particularly if associated with a hematoma and increase in volume on 5-minute delayed images, indicates active hemorrhage. Splenic artery pseudoaneurysms are contained vascular injuries that appear as small round or oval lesions with attenuation identical to that of arteries on initial images, that decreases ( following arterial attenuation) on delayed images. Extravasation and pseudoaneu- rysm are indications for emergent visceral arteriography.
Most classification systems grade splenic injury based on the size and location of subcapsular or parenchymal hematoma, length and depth of any laceration, and the presence or absence of active bleeding. Injuries that involve the vascular hilum may require embolization or splenectomy to control hemorrhage. Absent life-threatening hemorrhage, nonoperative management is preferred.
Depending on hemodynamic stability, most grade I–III injuries, as well as some of higher grade, can be managed nonoperatively. Grade IV and V injuries may require either arteriography/embolization or splenectomy.
Splenic Injury Grading
Grade I Subcapsular hematoma involving < 10% of surface area, or laceration < 1 cm depth
Grade II Subcapsular hematoma involving 10–50% of surface area, intraparenchymal hematoma < 5 cm in diameter, or laceration 1–3 cm in depth not involving trabecular vessels
Grade III Subcapsular hematoma involving > 50% of surface area, intraparenchymal hematoma > 5 cm, any expanding hematoma, laceration > 3 cm depth or involving trabecular vessels, or ruptured subcapsular or parenchymal hematoma.
Grade IV Laceration involving segmental or hilar vessels with > 25% devascularization
Grade V Shattered spleen or hilar vascular injury with devascularization
Examples
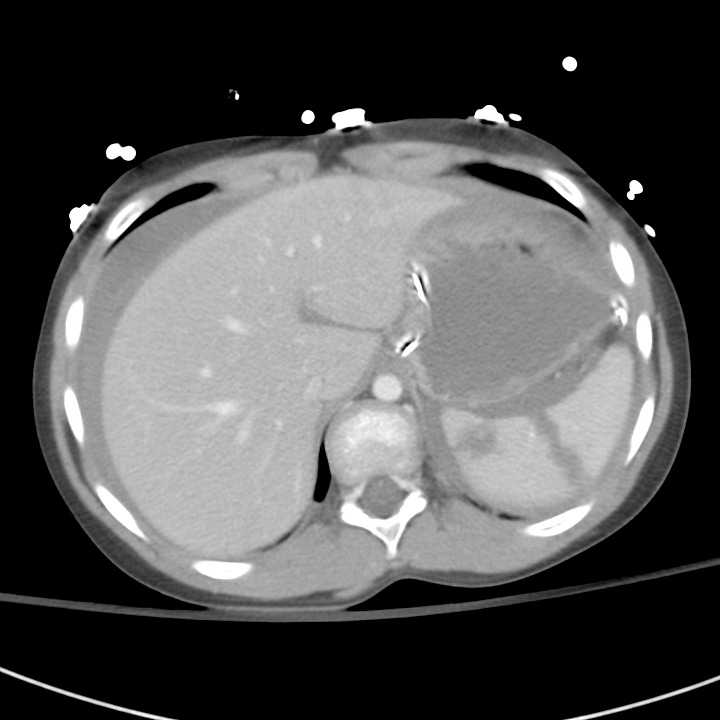

Grade III injury. Blunt trauma. A 5-cm laceration extends to the splenic hilum with extensive associated hemoperitoneum.
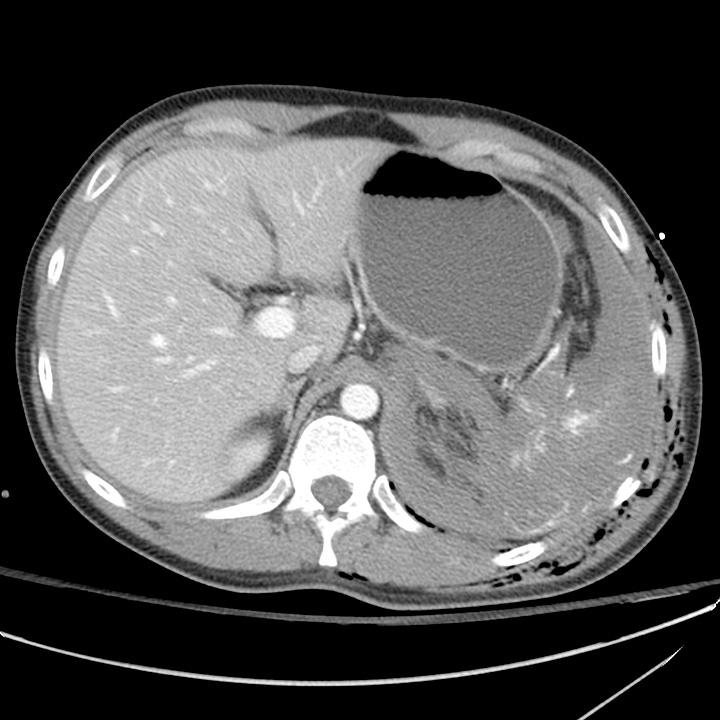
Grade III injury. Stab wound to flank. Deep laceration. No subcapsular hematoma or hemoperitoneum.

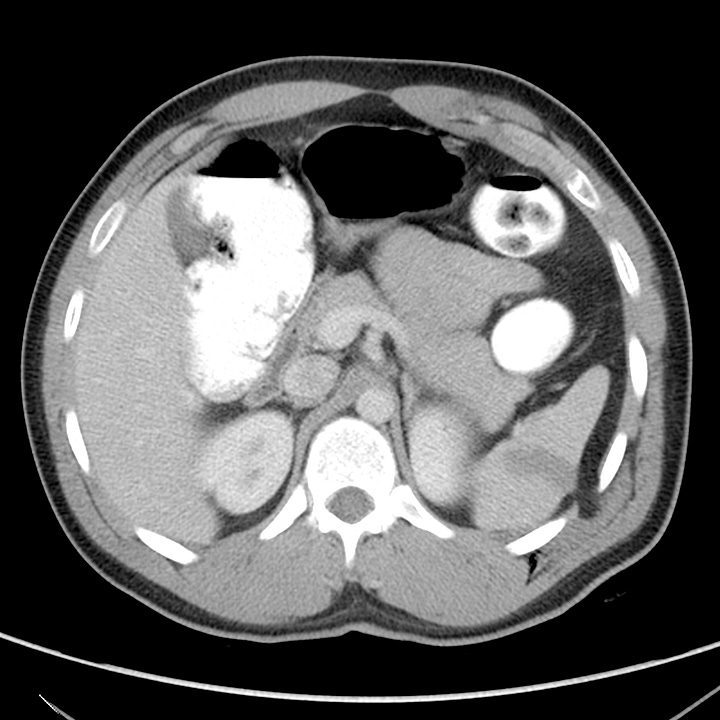
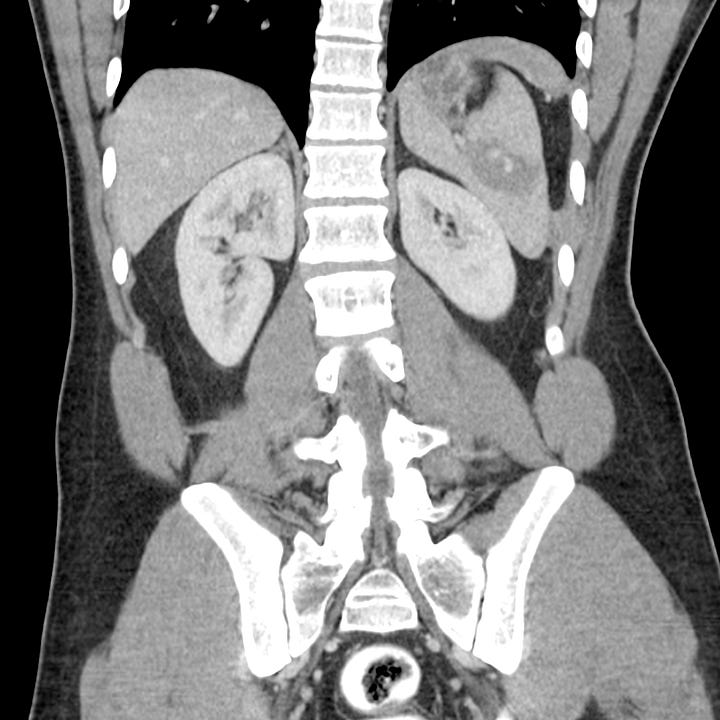
Grade V injury. Blunt trauma. Shattered spleen with associated grade V renal injury and extensive hemoperitoneum.



