Hemorrhage between the spinal dura and the adjacent vertebrae may complicate spinal fracture, minimal trauma, iatrogenic injury (lumbar puncture or epidural anesthesia), or it may be completely atraumatic. Spontaneous epidural hematomas occur in patients with blood dyscrasias, coagulopathies, thrombocytopenia, underlying neoplasm, vascular malformations and patients treated with antiocoagulants. These often manifest as severe localized subacute back pain with radicular radiation that mimics disk herniation. Weakness, numbness, and lower motor neuron signs may be present. In contrast to intracranial epidural hematomas, the source of bleeding is usually venous rather than arterial, and symptoms develop gradually as the hematoma enlarges over several days.
An acute spinal epidural hematoma appears on CT as a hyperdense mass in the spinal canal that extends over several vertebral levels. MRI has a greater sensitivity in detecting small epidural hematomas; in the first 24 hours, the hematoma is typically isointense on T1-weighted and hyperintense on T2-weighted images. As time progresses, it becomes hyperintense on both T1 and T2.


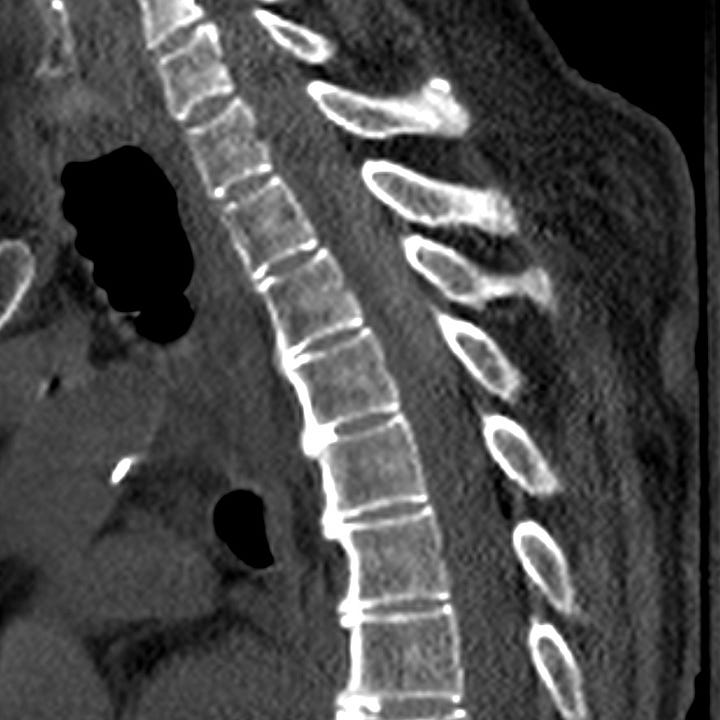
Spinal epidural hematoma in fused-spine hyperextension injury. High-attenuation dorsal, lentiform, intraspinous hematoma extending from C2–C3 to C6–C7. Widened C6–C7 disk space due to hyperextension injury and anterior ligamentous complex failure.

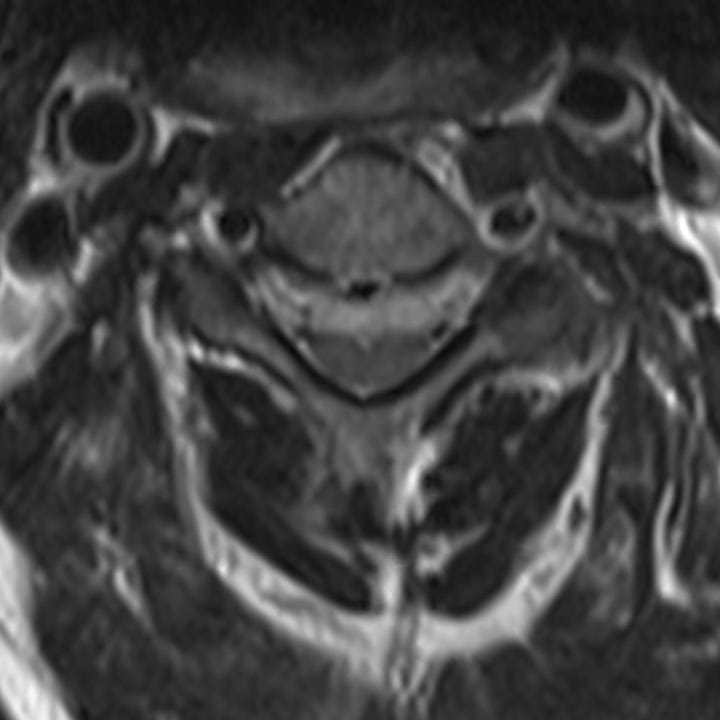
Atraumatic spinal epidural hematoma in an anticoagulated patient with syncope and acute weakness. Subtle, mixed-attenuation epidural collection dorsal to the lower cervical spinal cord on sagittal reformation. A blood-serum level within the hematoma is evident on the axial image dorsal and to the left of the cord.
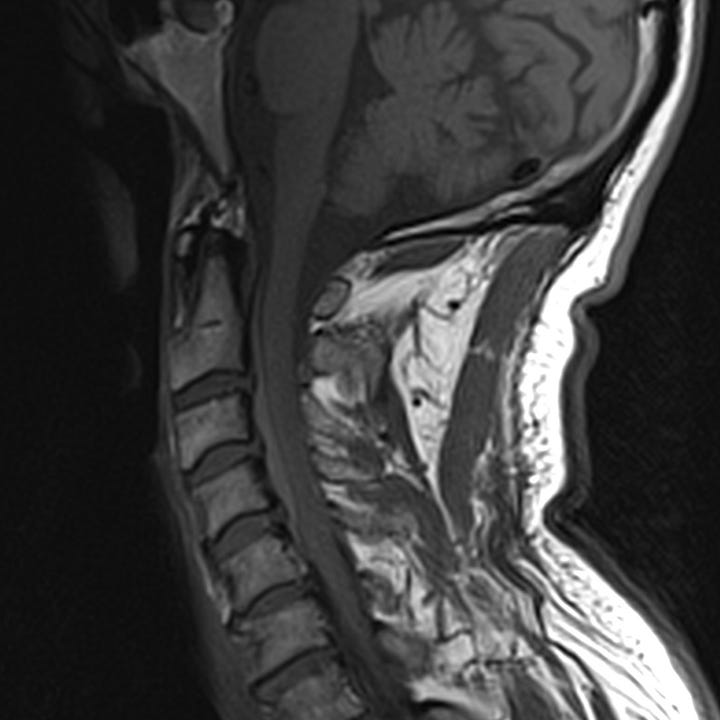
Spontaneous cervical spinal epidural hematoma in patient with acute unilateral upper and lower extremity weakness (MRI). Axial T2 weighted image shows a hyperintense epidural collection anterior to the cord that compresses the thecal sac. Sagittal T1-weighted image shows slightly hyperintense anterior epidural collection that extends over several levels.
Patients with severe or progressive neurologic deficits require surgical intervention, usually with laminectomy and clot evacuation. If the hematoma is small and deficits are minor or stable, patients can often be managed with observation and frequently achieve complete recovery.



