Respiratory distress syndrome (RDS) is an acute condition seen in children born before the lungs produce adequate surfactant to maintain alveolar expansion; neonates younger than 32 weeks gestational age or who weigh less than 1,200 grams. Symptoms are usually evident within hours of delivery and include cyanosis, tachypnea, expiratory grunting, nasal flaring, and substernal and intercostal retraction. Other risk factors include maternal gestational diabetes, prenatal asphyxia, and multiple gestations.
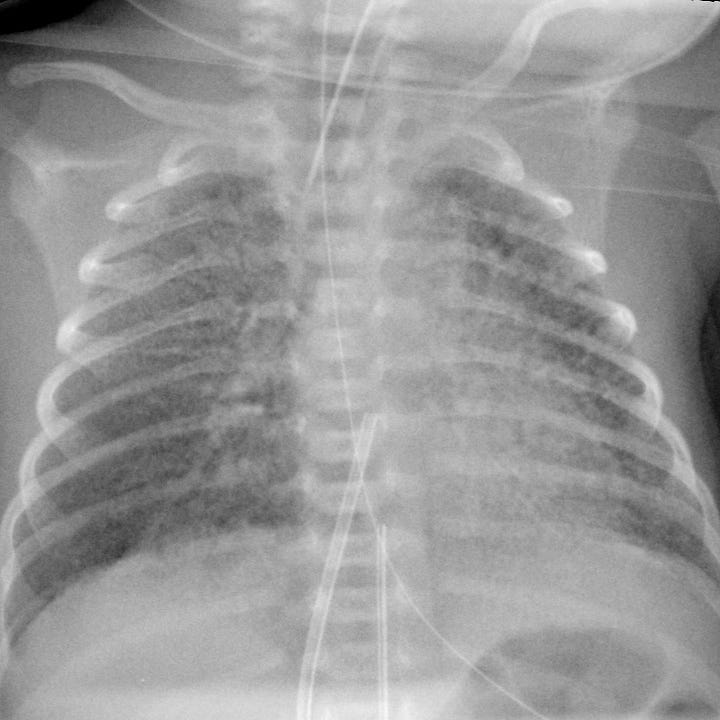
Radiographs show a bell-shaped thorax with a fine granular, or “ground glass,” pulmonary appearance, often with air bronchograms.


Lung disease of prematurity. Diffuse ground glass opacity involving all lung zones.
Management consists of administration of artificial pulmonary surfactant, supplemental oxygen, early use of continuous positive airway pressure and, if necessary, supportive ventilation. Antenatal steroids can be used to accelerate pulmonary maturity, and has reduced the incidence and severity of neonatal respiratory distress syndrome.
Complications are related to ventilation and barotrauma, and include pulmonary interstitial emphysema, pneumothorax, and bronchopulmonary dysplasia.

Pulmonary interstitial emphysema. Subsequent examination for the above patient. Endotracheal tube, umbilical arterial and umbilical venous catheters have been placed. New linear lucencies in the lung parenchyma correspond to air that has dissected from the alveoli into the pulmonary interstitium.
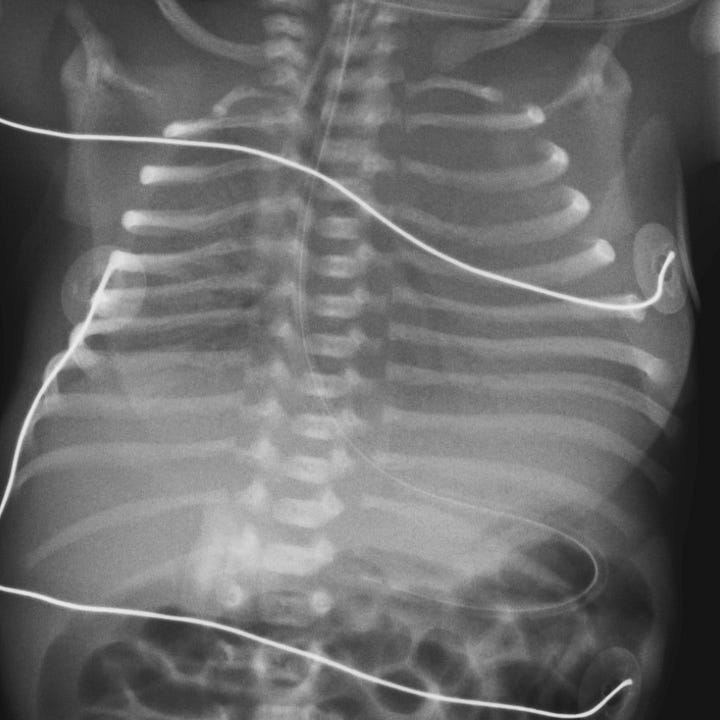

Pneumothorax complicating RDS. Initial study shows a bell-shaped thorax with diffuse ground glass opacity, air bronchograms and endotracheal and nasogastric tubes. Subsequent radiograph shows a left-sided pneumothorax and interval placement of umbilical arterial and venous catheters.



