Pneumothorax
Chest
Pneumothorax refers to the intrapleural accumulation of air due to a visceral pleural tear. It can be caused by barotrauma, rupture of a peripheral bleb or other pulmonary lesion, and blunt or penetrating chest trauma. Especially in traumatic pneumothorax, a one-way valve effect allows air to accumulate on inspiration that cannot exit the pleural space on expiration. Untreated, intrapleural pressure on the side of the pneumothorax can exceed atmospheric and contralateral intrathoracic pressure; mediastinal compression and displacement leads to reduced cardiac output and systemic perfusion. Clinical signs include diminished breath sounds over the affected hemithorax, tachycardia, hypotension, jugular venous distention, and contralateral tracheal shift.
Smoking is the most common risk factor for spontaneous pneumothorax, which is usually due to rupture of a subpleural bul- la. Primary pneumothorax typically occurs in persons under the age of 35 and is not associated with underlying lung disease. Secondary pneumothorax can occur in the settings of chronic obstructive pulmonary disease, asthma, cystic fibrosis, interstitial lung disease, and malignancy. Patients typically present with acute pleuritic chest pain and dyspnea, but many are only minimally symptomatic.
On upright PA radiographs, a fine, dense line corresponds to the visceral pleura and divides the lucent, air-filled lung from air in the pleural space. Pulmonary vessels and other lung markings are not visible lateral to the visceral-pleural line. The heart and mediastinum are often normal in position but may be displaced to the opposite side in tension pneumothorax.
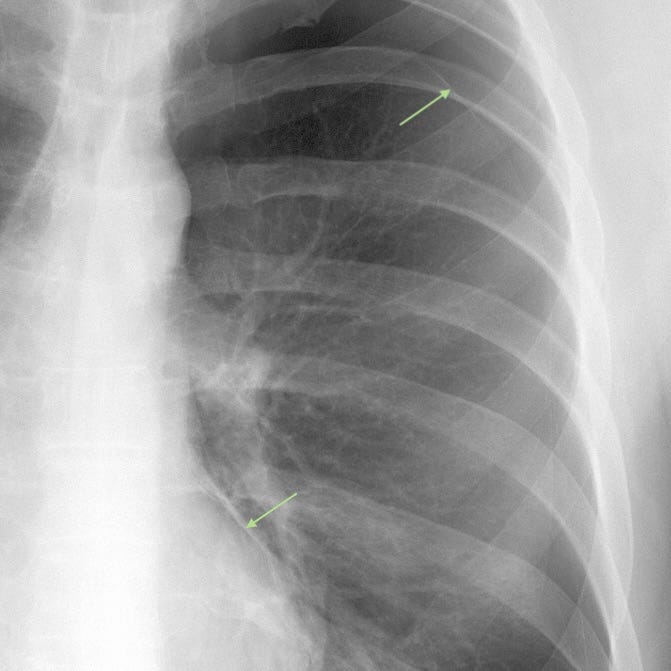
Tension pneumothorax. Left pneumothorax and pneumomediastinum (arrows). Subtle visceral-pleural line.
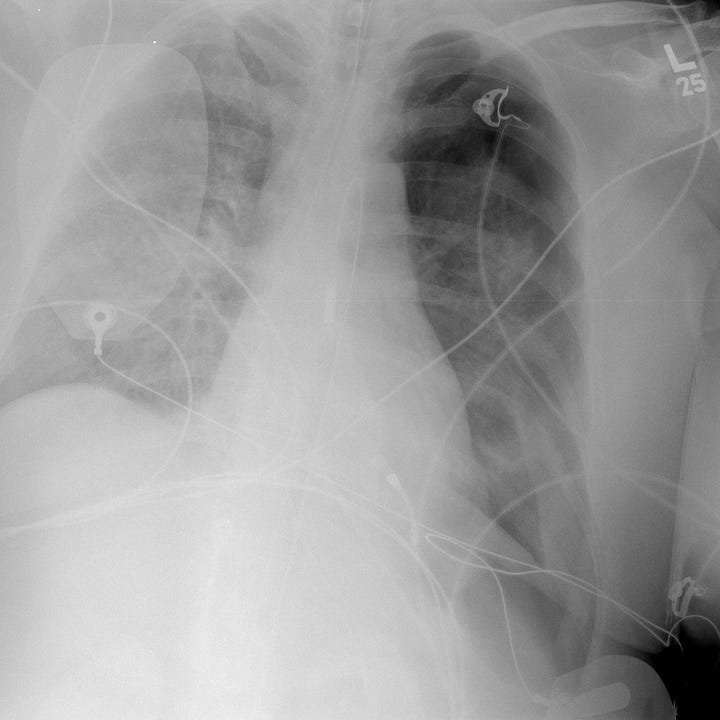
Tension pneumothorax. Same patient as above with left pneumothorax and pneumomediastinum. Mild left to right mediastinal shift.
Supine, portable radiographs obtained in trauma patients often do not show pneumothoraces even when present, partly because air in the pleural space lies anterior, rather than lateral to the lung, and the pleura is imaged en face rather than tangentially. Thoracic hyperlucency that extends over the lateral costophrenic angle and upper abdomen is referred to as the “deep sulcus” sign and is a useful but indirect finding in acute trauma.

Deep sulcus sign on supine portable radiograph. Initial study (left) shows diffuse bilateral airspace opacity due to cardiogenic edema. Subsequent supine radiograph (right) shows left sided pneumothorax with deep sulcus sign.
Ultrasound can identify pneumothorax in the trauma setting, but findings are often subtle. The normal lung shows mobile dotlike echoes as the visceral pleura moves against the parietal pleura with respiration. In pneumothorax these mobile echoes are not seen.
Skin folds can simulate the appearance of a pneumothorax and are seen exclusively on portable AP chest radiographs. When the detecting plate is placed behind the patient, redundant skin can fold against the plate, causing an air–soft tissue interface external to the patient and will appear as a dense edge against more lucent lung usually containing visible peripheral vessels.
In patients with hypoxia or vascular collapse, treatment should not be delayed while awaiting chest radiograph. A 14–16 gauge intravenous catheter can be inserted, either in the second anterior intercostal space in the midclavicular line or in the fifth intercostal space on the anterior axillary line, before a larger chest tube can be placed.