Pancreatic cysts are usually asymptomatic and incidental. Most are benign or indolent and include serous cystadenomas, mucinous cystic neoplasms, intraductal papillary mucinous neoplasms (IPMN), and pseudocysts. Ductal adenocarcinomas represent about 2.5% of incidentally discovered pancreatic cysts, and mucinous neoplasms, which have a malignant potential, represent about 55%.

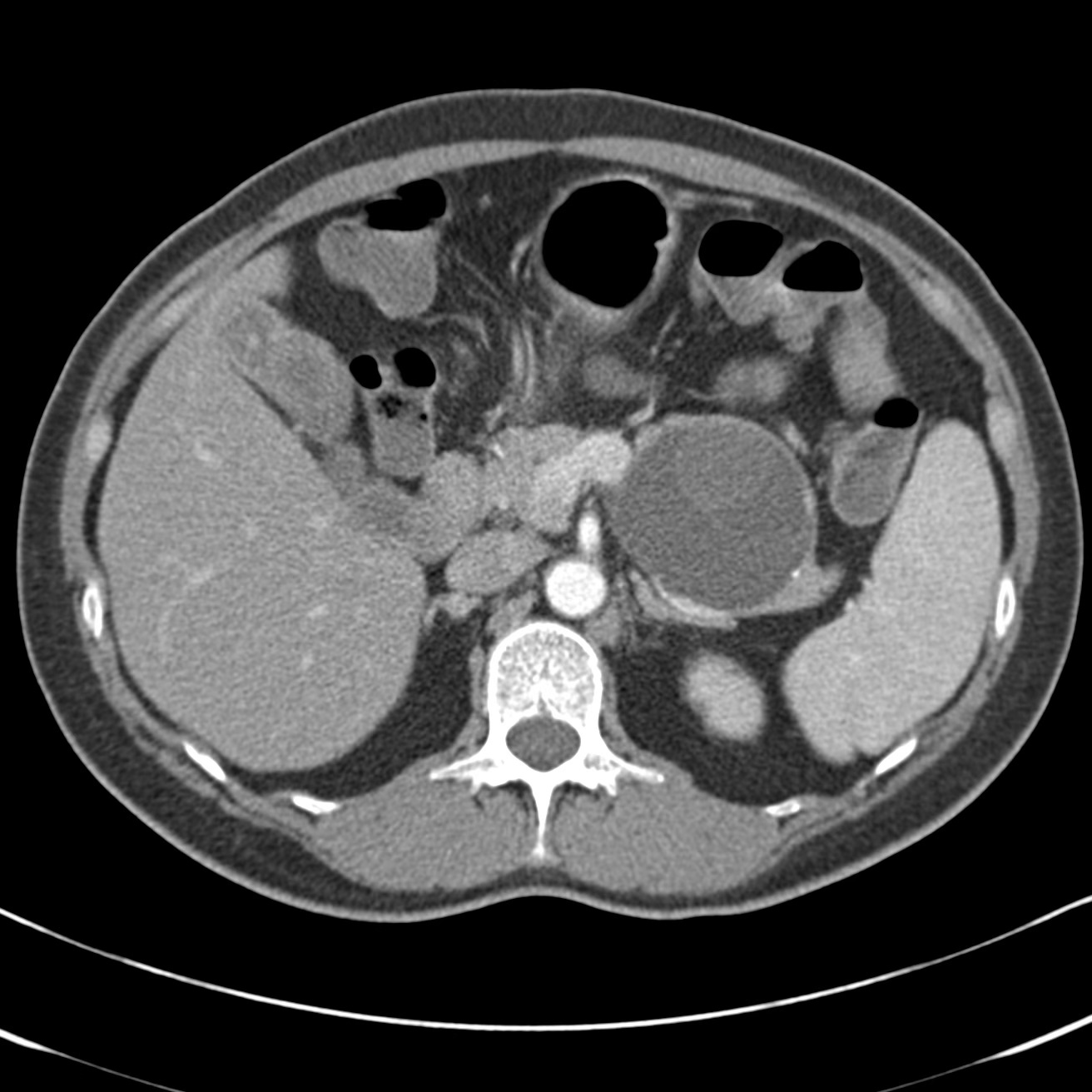
Intraductal papillary mucinous neoplasm. ~ 2.5-cm cystic mass in the pancreatic head with associated pancreatic duct dilatation
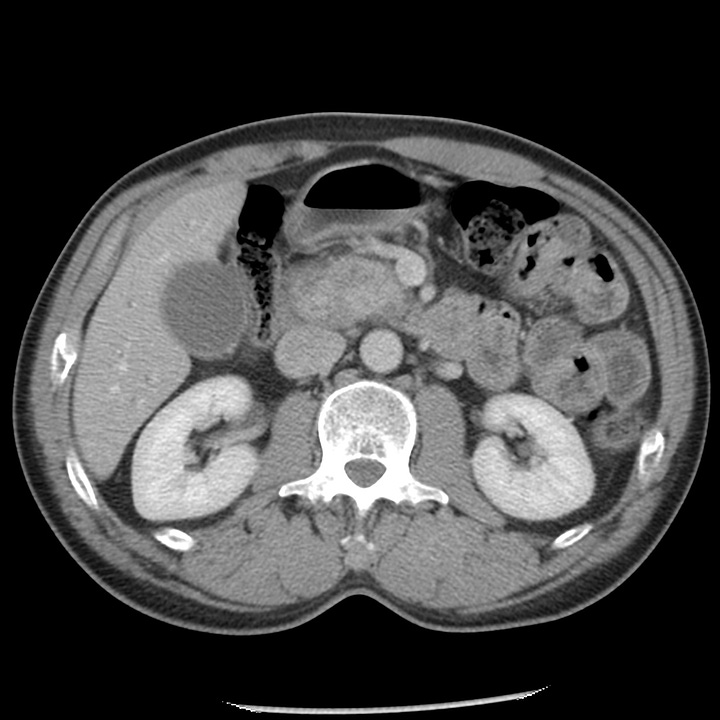
Serous cystadenoma. Simple 5-cm cyst in the pancreatic tail.
Mucinous cystadenoma. Complex cyst in the pancreatic tail with internal septations and intermediate- attenuation component.
Simple cysts < 2 cm should be reimaged in one year and, if stable, are considered benign.
Simple cysts 2–3 cm (and those that have grown from < 2 cm) should be characterized by MRI. Uncharacterized masses should be followed yearly. Cysts consistent with branch-duct IPMNs should be followed every 6 months for 2 years and annually thereafter. Cysts consistent with serous cystadenomas should be followed every 2 years and resection considered if they grow to > 4 cm.
Cysts > 3 cm should be characterized by MRI; most should be considered for cyst aspiration and resection depending on risk and comorbidities. Serous cystadenomas should be considered for resection when they reach 4 cm.
Solid pancreatic masses include true neoplasms, primarily adenocarcinoma and neuroendocrine tumors. Nonneoplastic conditions that can mimic tumors include autoimmune pancreatitis, intrapancreatic spleen, or sarcoidosis. Solid tumors and cysts with solid components should generally be resected.
Pancreatic adenocarcinoma is the most common primary pancreatic malignancy and affects patients in the seventh and eighth decades. Risk factors include smoking, alcohol, male gender, obesity and predisposing genetic syndromes including Peutz-Jehgers syndrome, ataxia telangiectasia, and presence of BRCA1 and 2 genes.
Pain, jaundice, and weight loss are typical presenting signs and symptoms. Unfortunately, most tumors are unresectable at the time of diagnosis, due to advanced local disease, hepatic metastases or peritoneal metastases. Five-year survival is ~ 5%.
Thin section CT in both arterial and portal venous phases is the best technique for evaluating solid pancreatic tumors, and most will appear as low-attenuation masses within the normally enhancing pancreas. Potentially resectable tumors show clear fat planes around the hepatic, celiac, and superior mesenteric arteries, tumor that does not abut the portal or superior mesenteric vein, and absence of distant metastases.

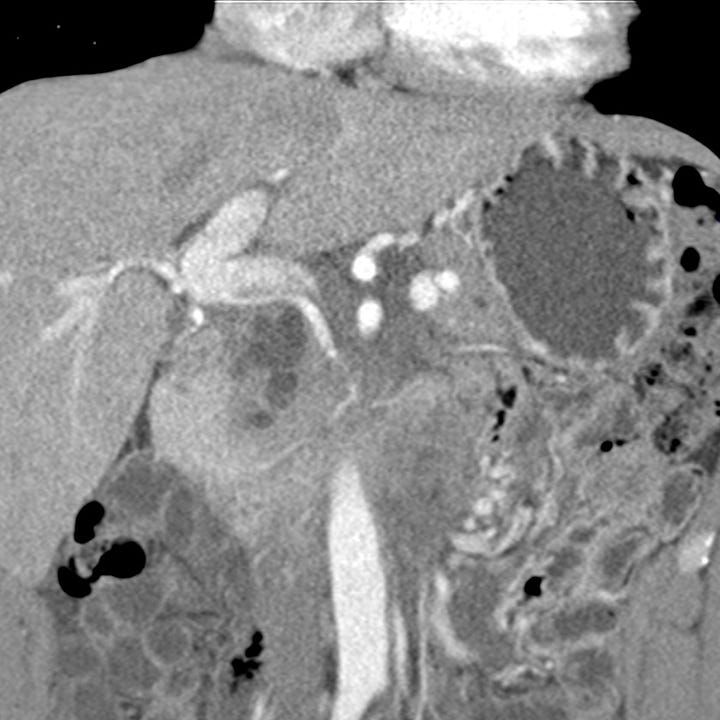
Pancreatic carcinoma. Solid, enhancing mass in head of pancreas with associated intra- and extra-hepatic biliary dilatation.