Direct ocular trauma in which the sclera is disrupted and vitreous humor leaks into the adjacent orbital tissue defines an open globe injury. Globe rupture may follow either blunt or penetrating trauma. In blunt trauma, it frequently occurs at intraocular muscle insertions, where the sclera is thinnest.
Although ophthalmoscopy is more sensitive for detection of small ruptures, periorbital soft tissue swelling can limit direct clinical evaluation, and globe rupture is often identified on CT obtained for face or head injury. The ruptured globe may appear small and irregular, or can have a flattened contour reminiscent of a “mushroom” or “flat tire.”
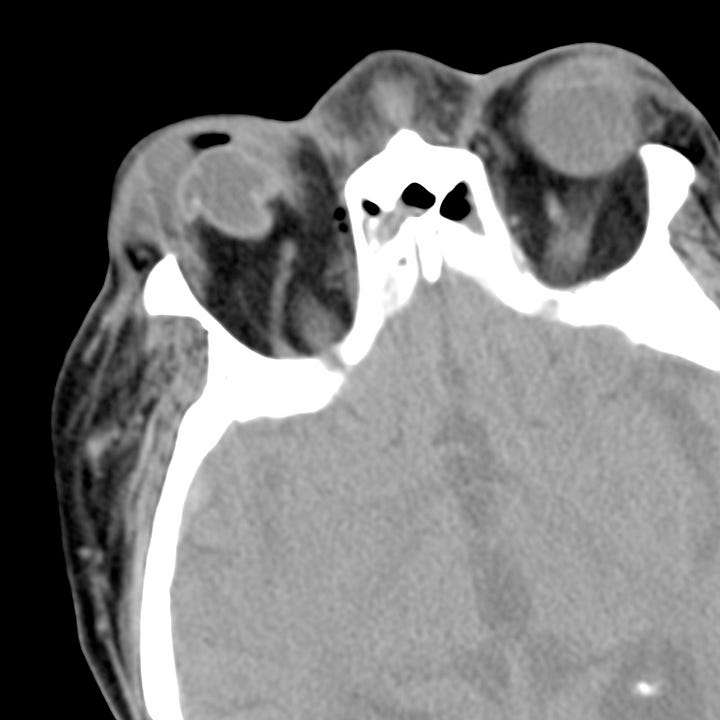
Globe rupture. Extensive right-sided preseptal periorbital hematoma. The right globe is distorted with a mushroom-like appearance. In the image on the right, a tiny linear density superolateral to the anterior globe is an extruded intraocular lens implant.
Some globe ruptures are inapparent on CT. In patients with an apparently intact globe, unilateral posterior lens subluxation (deep anterior chamber) or thickening of the posterior sclera are subtle signs of globe injury. More obvious CT findings include scleral discontinuity, intraocular air or hemorrhage, lens subluxation, intraocu- lar foreign bodies, and traumatic cataract.


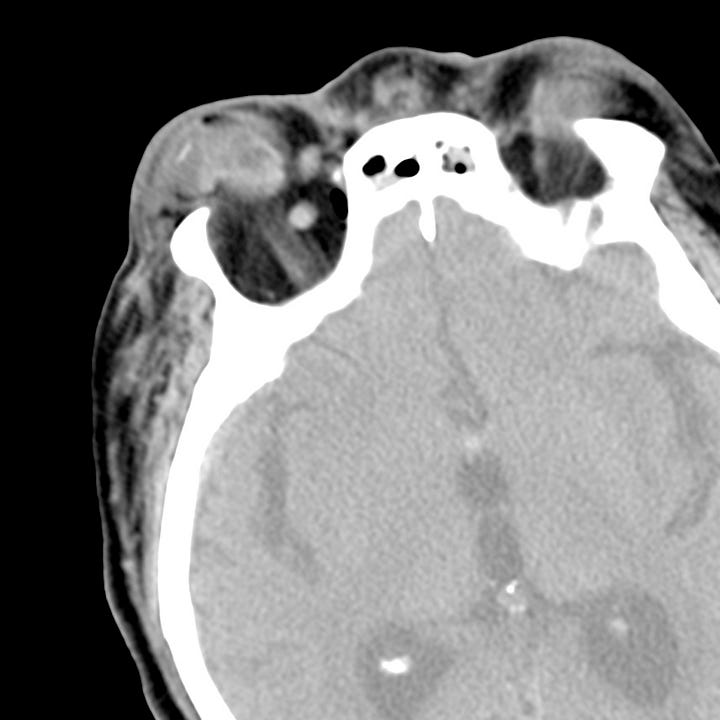
Globe rupture. The image on the left shows left globe posterior flattening and reduced volume. The lens is displaced from its normal position. The image on the right shows vitreous hemorrhage from drill-bit perforation with anterior globe flattening, and posterior vitreous versus choroidal hemorrhage.
Any traumatic orbital hematoma, and retrobulbar hematomas in particular, can injure the optic nerve as a result of increased intra-orbital pressure. The clinical presentation is variable, and symptoms related to hematoma formation may not manifest until several days after the acute injury.
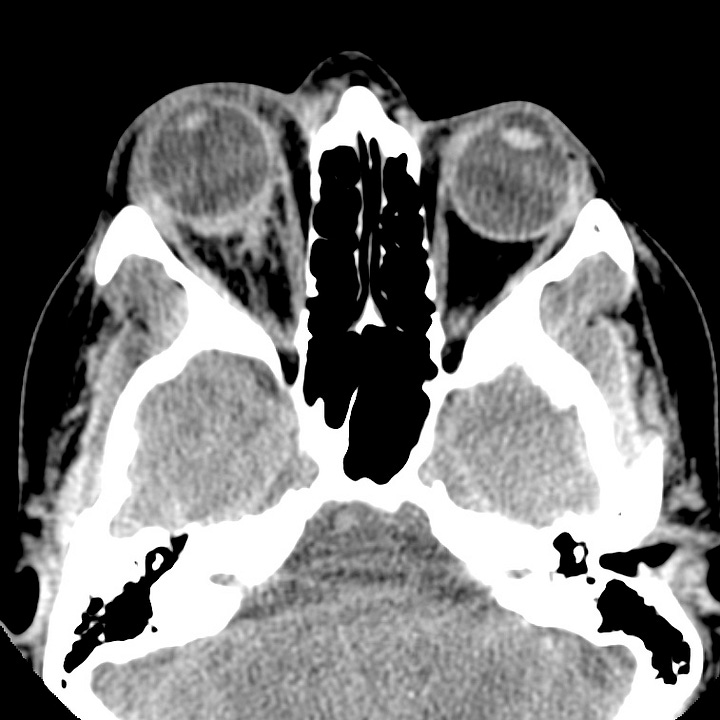

Intraorbital hematoma. Right intraconal and retrobulbar soft tissue stranding with associated mild proptosis. Normal globe dimensions.
CT identifies proptosis, stretching of the optic nerve, and “globe tenting,” in which the angle made by two tangents to the globe that intersect at the optic nerve head is less than 130°. While orbital hemorrhage and hematoma are uncommon, traumatic orbital compartment syndrome can lead to vision loss; in such cases prompt lateral canthotomy and cantholysis may prevent blindness.

