Neurocysticercosis
Brain

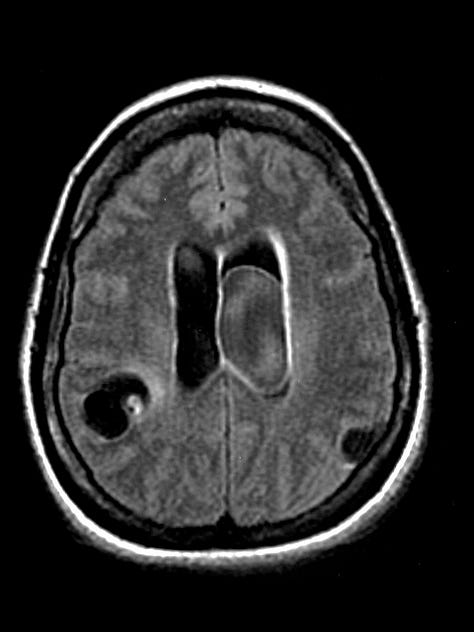
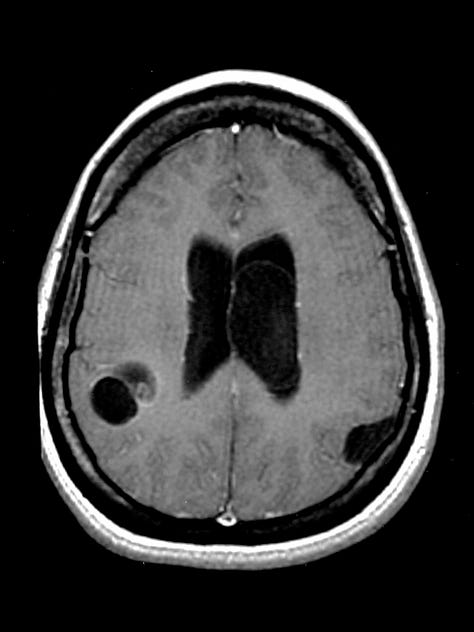
CT, Fluid Attenuation Inversion Recovery (FLAIR) MRI, and Post-gadolinium T1 weighted MRI show parenchymal, subarachnoid, and intraventricular cysts. On the FLAIR image, a right parietal parenchymal cyst contains an encysted scolex. An intraventricular cyst shows signal with higher intensity than simple CSF.
Cysticercosis—systemic infestation by the larval form of the pork tapeworm Taenia solium—is endemic to Central America, South America, Asia, and Africa. The incidence in the United States has been steadily rising as a result of immigration and international travel. Infestation can involve almost any tissue, and neurocysticercosis is the leading cause of adult-onset epilepsy worldwide. Obstructive hydrocephalus, meningoencephalitis, stroke, headache, and altered mental status are other manifestations.
Clinical and imaging findings depend on the stage of the disease. The encysted larva enjoys immunologic invisibility as long as it is alive, and most patients are asymptomatic at this stage. When the larva dies, it elicits an immune reaction that can lead to focal cerebritis and seizure.
The encysted larva with surrounding cerebritis appearson CT as a low attenuation lesion with peripheral enhancement and surrounding vasogenic edema. As acute inflammation resolves, the cyst retracts and appears as an enhancing parenchymal nodule with diminishing adjacent edema. Over time, the lesion calcifies.
The racemose form of neurocysticercosis consists of thin-walled “grapelike” cysts in the subarachnoid, intraventricular, and cisternal CSF spaces. Because the CT attenuation of unruptured cysts corresponds to that of CSF, an intraventricular cyst may be nearly undetectable and a subarachnoid cyst may be indistinguishable from a small arachnoid cyst. MRI imaging with FLAIR sequences readily differentiates the higher-signal cyst contents from normal CSF. Cysts that obstruct normal CSF flow can cause acute hydrocephalus


Let's see....
1. Yes, when cysticercosis involves muscle it typically presents as either cysts or rice like linear calcifications (end result of dead cysts, as in the brain)
2. I think that plate like stranding in the lungs is so common that it would be hard to use this finding as a diagnostic discriminator. Lung nodules have been described in cysticercosis but I haven't seen "plate-like" stranding, which usually means sub segmental atelectasis or scar.
3. I assume that the best diagnostic test for following up a lesion after treatment is the one used to detect it in the first place; CT or MRI for intracranial disease, ultrasound or MRI for soft tissue cysts.
4. Not sure about the current clinical guidelines for treatment. Usually antihelminths are used in symptomatic patients, so it depends on the clinical situation. I'd check the internet for the latest recommendations.
Thanks for the questions, and for subscribing.
I have questions on neurocysticercosis. Besides the cysts/tumors in brain, can the parasites present as a linear lesion? Another question, Can plate-like stranding in lung tissue be caused by cysticercosis? And finally, what is best diagnostic for this parasite after 4 months of treatment with ivermectin and fenbendazole? Is Praziquantel advised in elderly even with risk of seizures when no incidence of seizures?