Necrotizing enterocolitis (NEC), refers to segmental ischemic intestinal necrosis seen in premature and low-birth-weight infants. It usually develops in the first 2-10 days of life and reflects a combination of infection, ischemic injury, and incompletely developed immunity. Feeding intolerance, bile-stained vomitus, abdominal distention, and gross or occult blood in stool are typical presenting signs. Predisposing factors include prematurity, congenital heart disease, birth anoxia, and sepsis.
Abdominal radiographs are often nonspecific and may only show ileus or bowel wall edema with thumbprinting. Pneumatosis intestinalis, when present, appears as a mottled, granular appearance to the bowel and is considered diagnostic. Portal venous gas and pneumoperitoneum indicate severe disease and perforation, respectively.
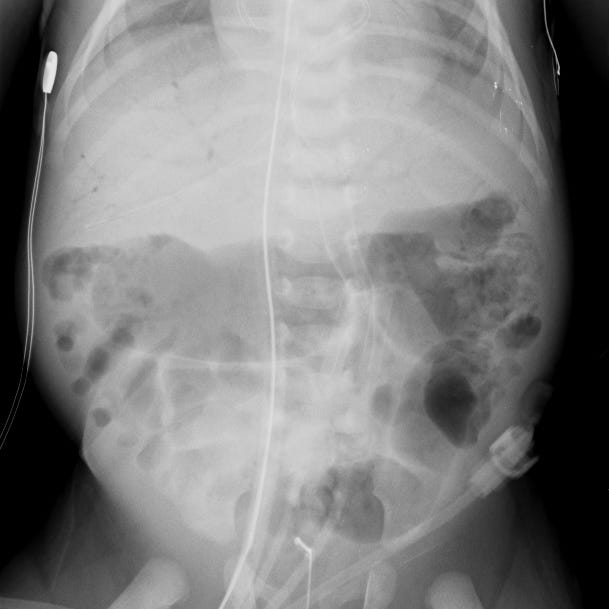

Necrotizing enterocolitis with pneumatosis intestinal and portal venous gas. Intramural gas within the bowel causes portions of the left colon to appear granular or mottled. The right image (detail) shows tubular lucencies over the liver corresponding to gas in the portal veins.
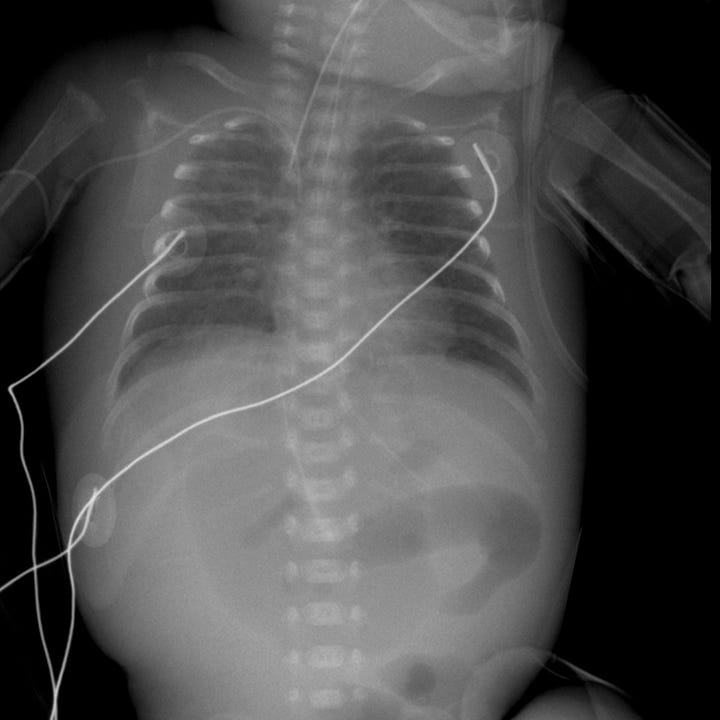
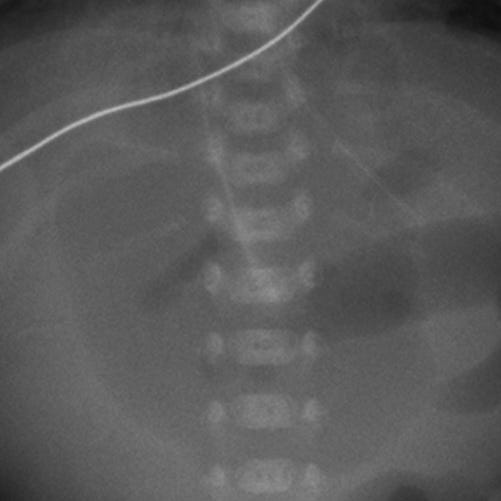
Bowel perforation due to necrotizing enterocolitis. Large oval lucency over the upper abdomen on supine radiograph. The right image (detail) demonstrates a vertically oriented linear density that corresponds to the falciform ligament outlined by free intraperitoneal air. Perforation may also be diagnosed by identifying air on both sides of the bowel wall or finding nondependent free air on a decubitus (horizontal beam) radiograph.
Most cases of NEC are managed medically with bowel rest, placement of an orogastric tube, fluid resuscitation, and broad-spectrum antibiotic treatment. Surgery is reserved for patients with clinical and imaging evidence of perforation.

