Necrotizing enterocolitis (NEC), segmental mucosal or transmucosal ischemic necrosis of the intestine, is commonly seen in premature and low-birth-weight infants. NEC reflects a combination of infection, ischemic injury, and incompletely developed immunity. Predisposing factors include prematurity, congenital heart disease, birth anoxia, and sepsis. NEC usually develops in the first 2–10 days of life, with an incidence inversely proportional to gestational age. Clinical findings are often nonspecific but include feeding intolerance, vomiting, bile-stained vomitus, abdominal distention, and gross or occult blood in stool.
Abdominal radiographs may show ileus, bowel wall edema with thumb-printing, and loss of the normal polygonal gas shape within the dilated intestine. Pneumatosis intestinalis is considered pathognomonic, and portal venous gas and pneumoperitoneum indicate severe disease and perforation, respectively.
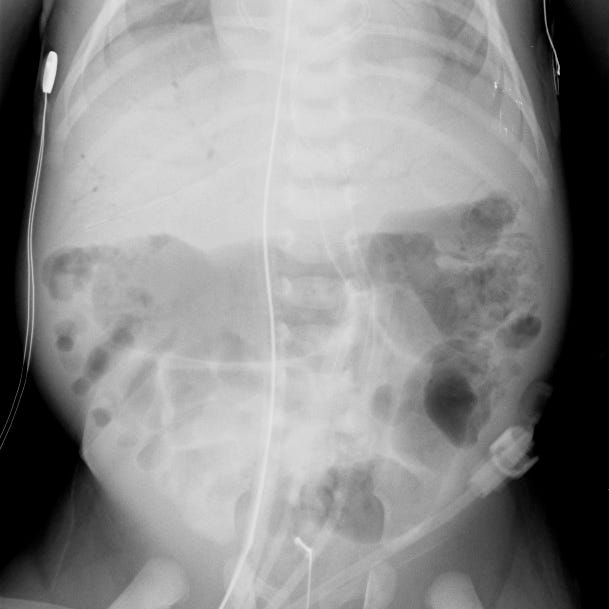
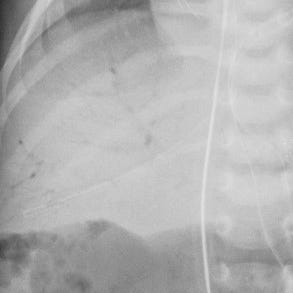
Necrotizing enterocolitis. Left colon intramural gas results in mottled appearance. Detail shows portal venous gas.
Medical management consists of bowel rest, orogastric tube placement, fluid resuscitation, and broad-spectrum antibiotics. Surgical intervention is reserved for patients with clinical and imaging evidence of perforation. On the supine radiograph, free air is indicated by finding gas on both sides of the bowel wall, or clearly visualizing the falciform ligament. Suspected free air can be confirmed on decubitus radiograph.

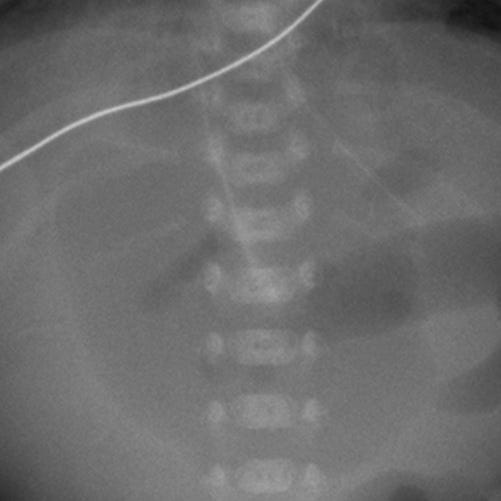
Bowel perforation in newborn. Large oval lucency over upper abdomen with linear density overlying the spine that corresponds to the falciform ligament outlined by free intraperitoneal air.

