Acute sinusitis, inflammation of the paranasal sinus mucosa, may be allergic or can be due to viral, bacterial, or fungal infection. The diagnosis is based upon the entirely clinical findings of facial pain and tenderness, postnasal discharge, congestion, and anosmia. Imaging is not indicated for acute sinusitis but may be obtained to evaluate an atypical headache or to diagnose the uncommon complications of untreated or inadequately treated sinusitis which include facial or orbital cellulitis, cavernous sinus thrombosis, subdural or epidural empyema or cerebritis/brain abscess. If a CT is obtained, acute uncomplicated sinusitis usually appears as fluid within a sinus.
Invasive sinusitis is associated with bone erosion and inflammatory disease that extends into the adjacent facial soft tissues. Invasive fungal sinusitis, the most common variety, is a disease of immunocompromised patients, most commonly diabetics, neutropenic patients on chemo- therapy, or patients with advanced AIDS. Clinical findings vary but include fever, facial pain, epistaxis, and nasal congestion. Infection that extends from the sinus into the orbit can lead to visual deterioration, proptosis, diplopia, and pain. Cranial nerve III–VI dysfunction indicates cavernous sinus involvement.
On noncontrast CT, the involved sinuses are usually opacified, with hyperostotic or thinned walls, permeative bone changes, and intraorbital or deep facial fat stranding. Intracranial complications include epidural empyema, meningitis, cerebritis, vasculitis, mycotic aneurysm, and vascular thrombosis. Systemic antifungal therapy and surgical debridement are often necessary for successful management.
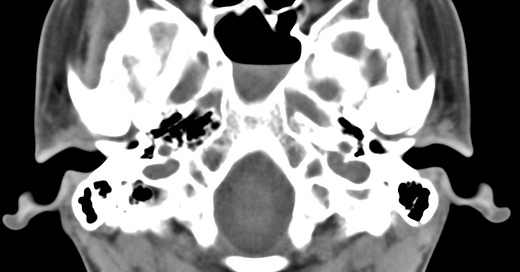
Acute sinusitis. Low-attenuation fluid within the sphenoid sinus. No associated hyperostosis.
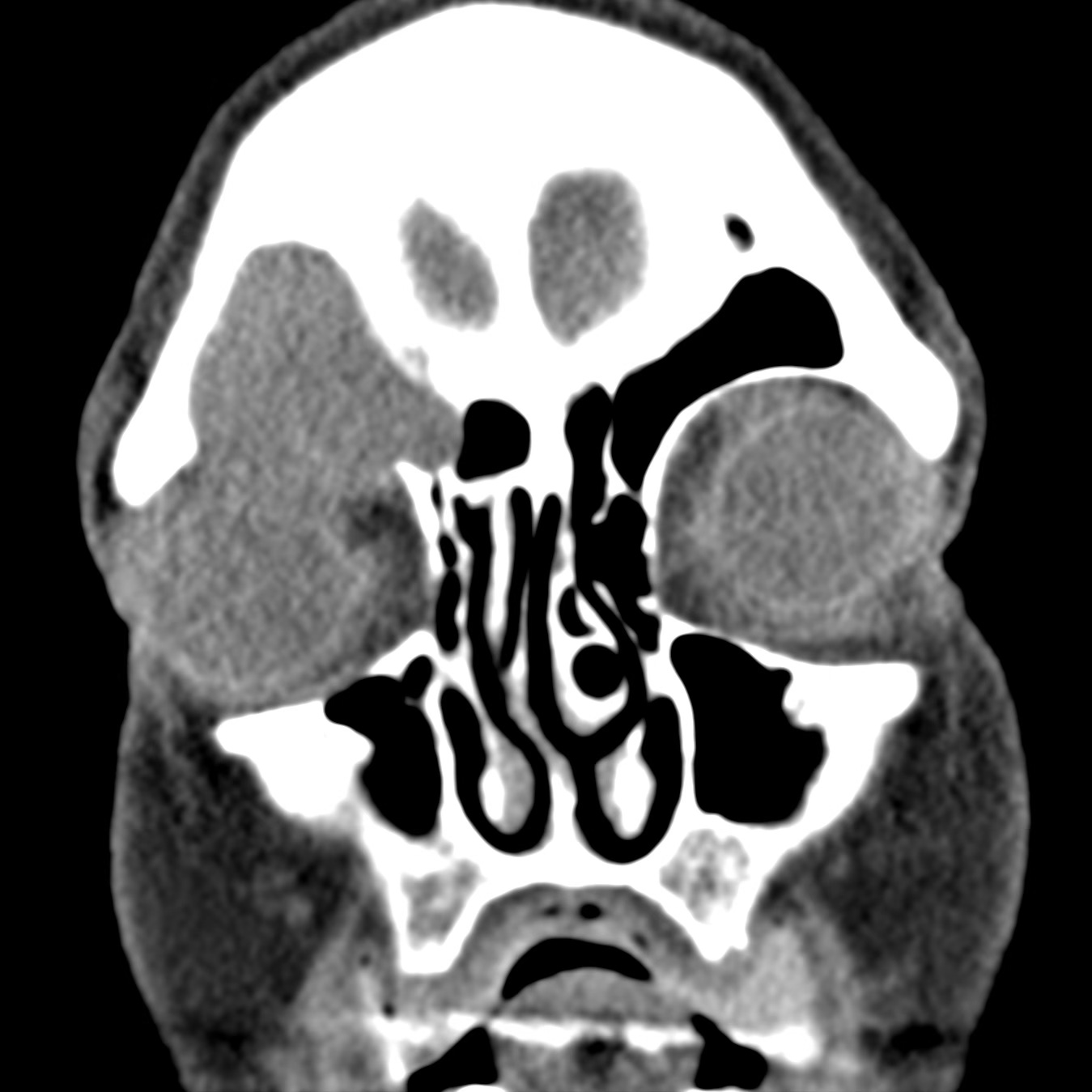
Invasive aspergillosis. The left maxillary sinus is opacified and enhancing inflammatory tissue extends through in the orbital floor to involve the inferomedial orbit.
Mucormycosis. Right ethmoid opacification with permeation and erosion of the ethmoid walls. Inflammatory tissue extends into the medial right orbit and preseptal soft tissues.
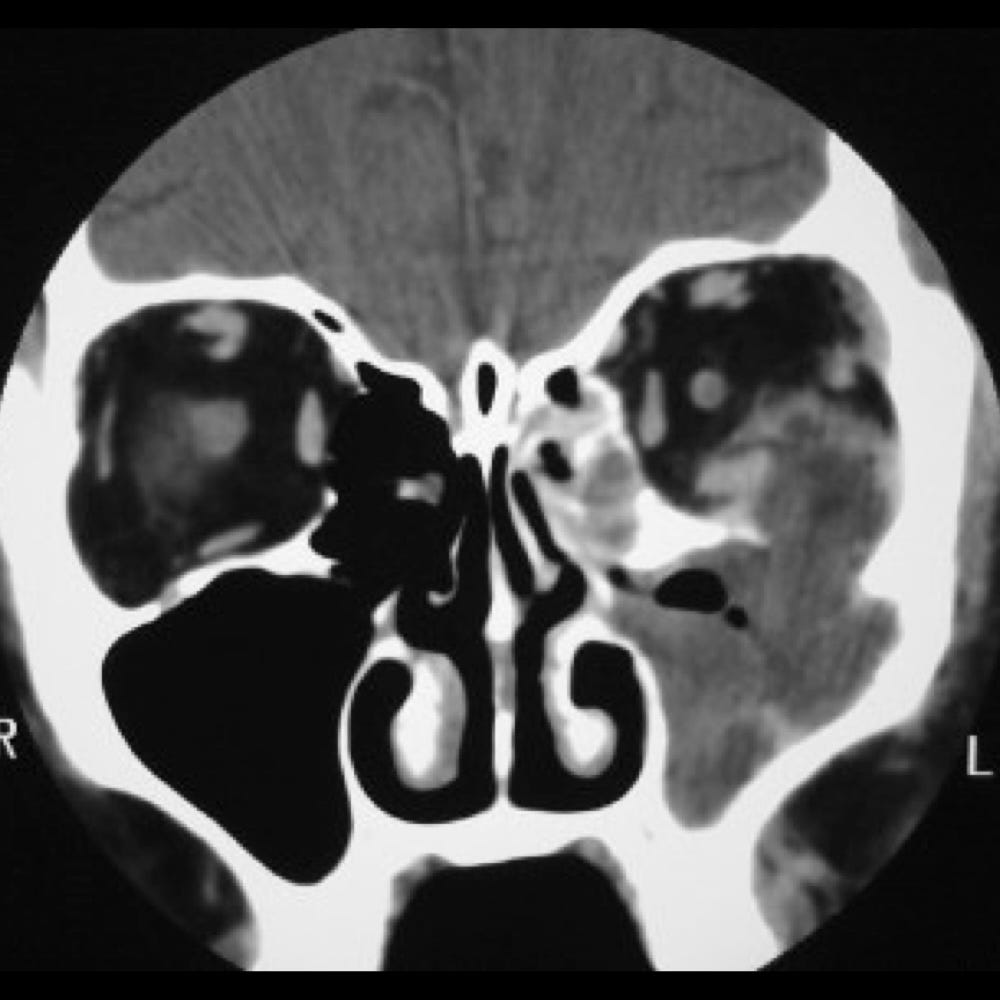
Sinus mucocele results from ostial obstruction due to chronic inflammation, allergies, trauma, or underlying neoplasm. Mucous under pressure accumulates in the sinus, expands and thins the walls, and can rupture into an adjacent sinus, the orbit, or the cranium. The frontal and ethmoid sinuses are most frequently involved, but any combination of paranasal sinuses may be affected. Clinical findings include facial deformity, exophthalmos, or diplopia from encroachment upon the adjacent orbit. Rupture of a mucocele can lead to cellulitis and facial or intracranial abscess.
CT imaging shows an expanded, completely opacified sinus with remodeling and thinning of at least one wall
Frontal sinus mucocele. Right frontal sinus opacification with smooth expansion and erosion of the anterior orbital roof. Associated inferior displacement of the globe. Intraorbital soft tissue infiltration indicates cellulitis.
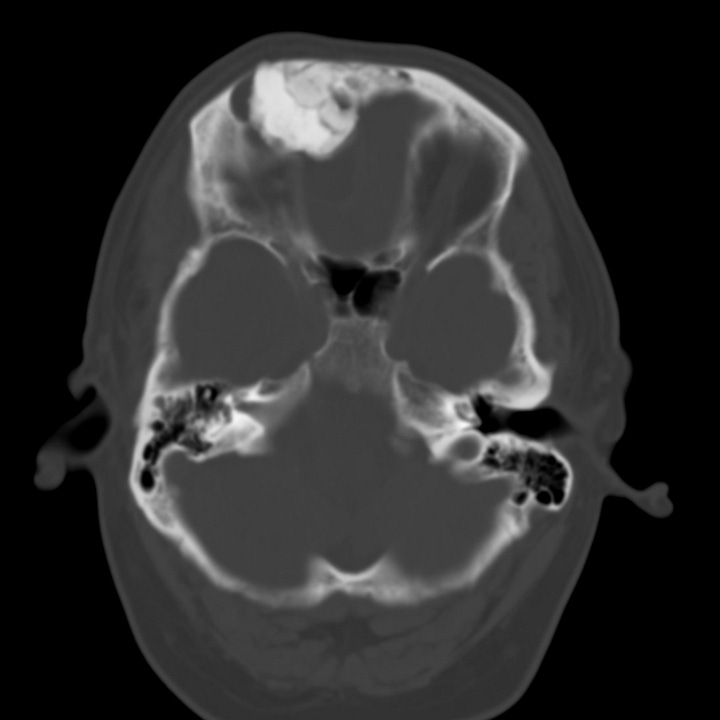
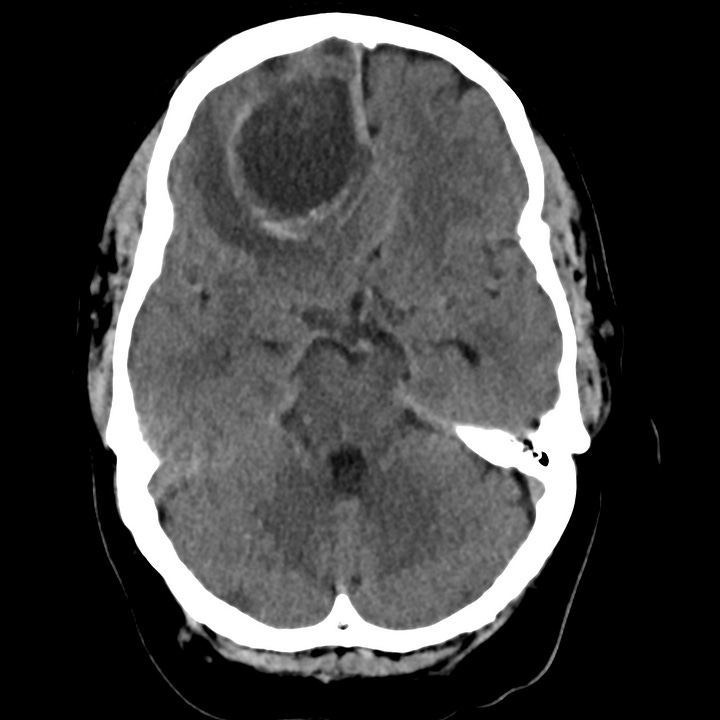
Brain abscess due to frontal sinus obstruction by osteoma. Large frontal sinus osteoma with small ruptured mucocele and complicating right frontal lobe brain abscess.