The liver is the second most frequently injured organ in the abdomen, and hepatic injury is the most common cause of death in abdominal trauma. Blunt injuries include subcapsular or intraparenchymal hematoma, contusion, capsular disruption, laceration, and biliary disruption. Penetrating injuries from stab or gunshot wounds are usually managed nonoperatively or by angioembolization.
Contrast-enhanced CT localizes and characterizes parenchymal injury and detects other associated visceral injuries. As in the case of splenic injury, angiography and embolization are indicated for active extravasation or hepatic artery pseudoaneurysm. An enhancing visceral lesion that matches arterial density on initial and delayed images indicates pseudoaneurysm. An area of contrast accumulation, particularly within a hematoma, indicates active extravasation.
The decision to operate or observe is dictated by the patient’s hemodynamic stability, the presence of active extravasation, or a decreasing hematocrit. Nonoperative management is generally preferred. High-grade injuries (IV–VI) should, if managed non-operatively, be reimaged in 7 to 10 days, or sooner if there is a change in the patient’s clinical status.
AAST Grading for Hepatic injury
Grade I
Subcapsular hematoma < 10% surface area or capsular tear < 1 cm depth
Grade II
Subcapsular hematoma 10–50% surface area, intraparenchymal hematoma < 10 cm diameter, or capsular tear, 1–3 cm depth and < 10 cm length
Grade III
Subcapsular hematoma >50% surface area, active bleeding, intraparenchymal hematoma > 10 cm diameter, or capsular tear > 3 cm depth
Grade IV
Intraparenchymal hematoma with active bleeding, parenchymal disruption involving either 25–75% hepatic lobes or 1–3 Couinaud segments within one lobe
Grade V
Parenchymal disruption involving > 75% of one hepatic lobe or > 3 Couinaud segments within one lobe, inferior vena cava laceration, or hepatic vein laceration
Grade VI
Hepatic avulsion
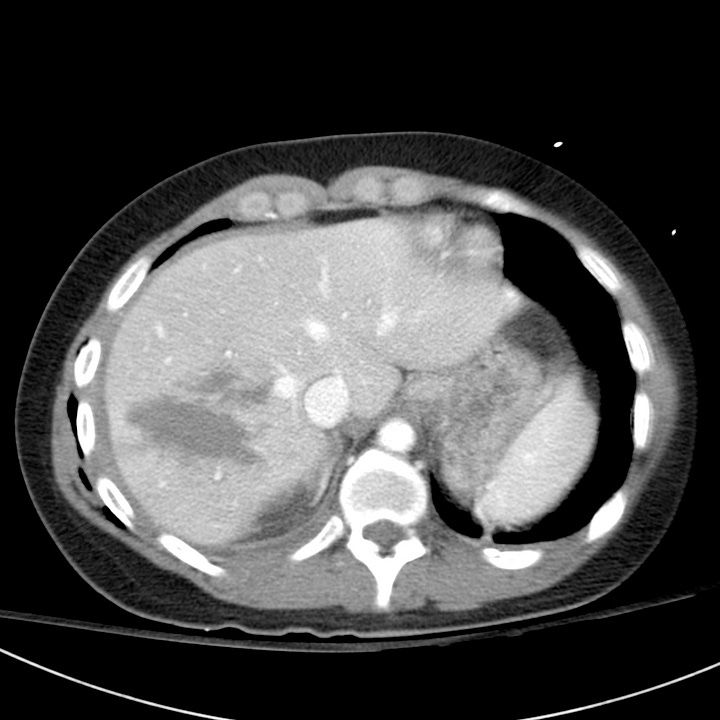
Grade II–III hepatic laceration, right lobe. ~ 8 cm laceration involving hepatic segments 5–8. Minimal perihepatic hematoma without active hemorrhage or pseudoaneurysm.


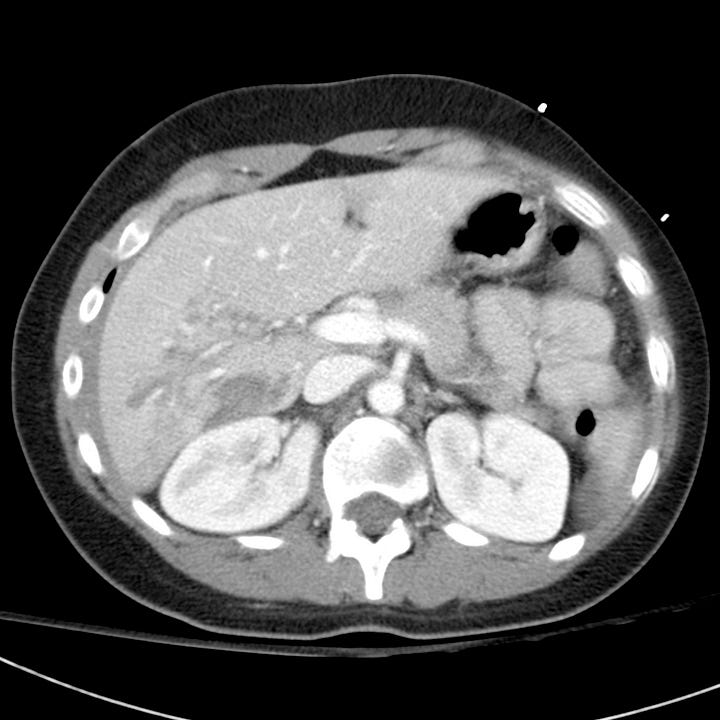
Grade III hepatic laceration, left lobe. Laceration involving the junction of the right and left hepatic lobes. Large associated mesenteric hematoma and hyperenhancing (shock) bowel.

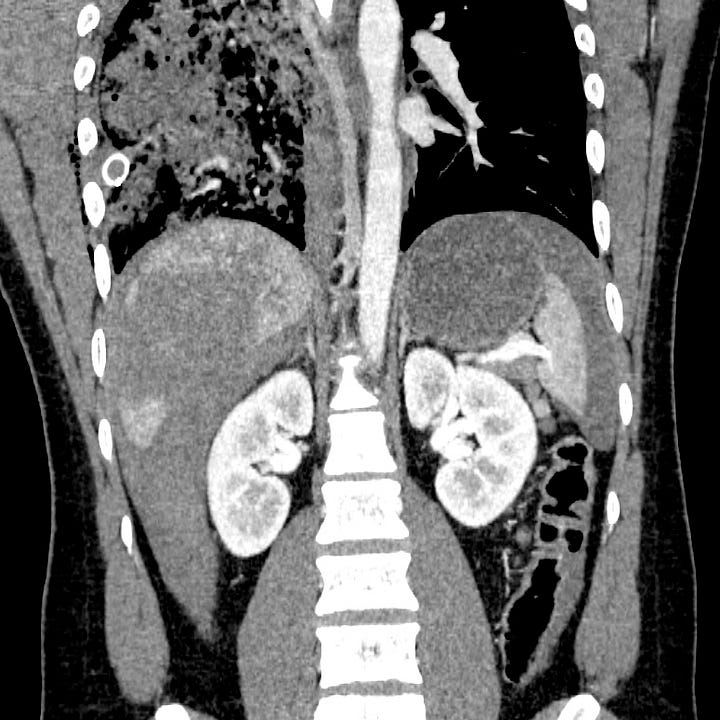
Hepatic parenchymal hematoma. Peripheral hematoma involving hepatic segments 5–8 (right hepatic lobe). Large amount of perihepatic and perisplenic intraperitoneal hemorrhage.

