Cerebral swelling, whether traumatic or non traumatic (intracranial neoplasm, infection, metabolic derangements, and hypoxic-anoxic injury), is often due to a combination of vasogenic and cytotoxic edema processes. In severe head trauma, cerebral tissue damage, often associated with systemic hypovolemia, hypoxia, and hypercarbia, disrupts normal auto-regulation and leads to a toxic cycle of elevated intracranial pressure, cerebral ischemia, and further tissue damage. Swelling localized to one cerebral compartment can cause subfalcine, transtentorial (uncal), or central herniation; vascular compromise; and ischemia.
CT findings include global sulcal effacement, slit-like ventricles, and compressed perimesencephalic and suprasellar cisterns. In head trauma, swelling is usually associated with other findings such as extra-axial hematomas, cerebral contusion, subarachnoid hemorrhage, and unilateral ventricular enlargement (trapping) on the side opposite any parenchymal or extra-axial hematoma.

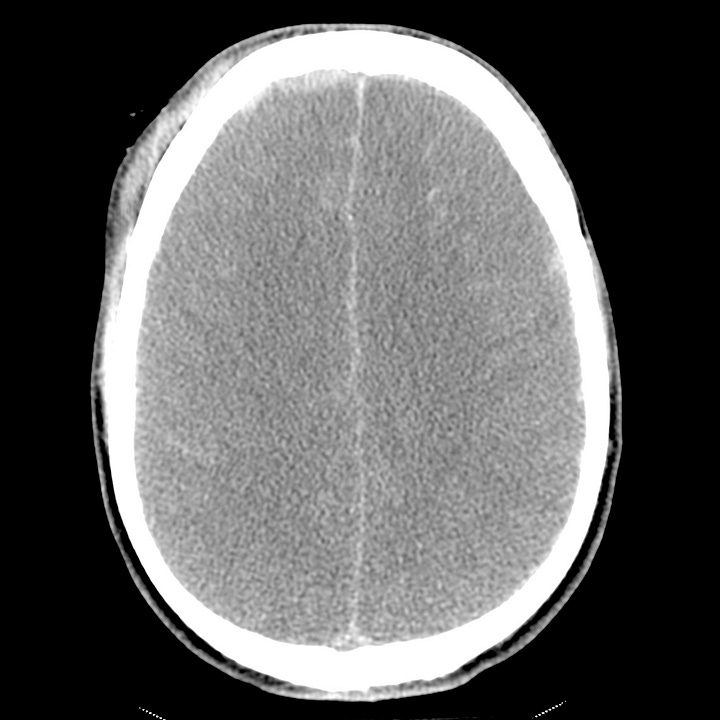
Traumatic cerebral swelling. Small right frontal extra-axial hematoma and diffuse traumatic subarachnoid hemorrhage. Global cisternal and sulcal effacement with poor gray-white differentiation. Associated right frontal scalp soft tissue swelling, orbital roof fracture, intra-orbital hematoma, and intra-orbital air.
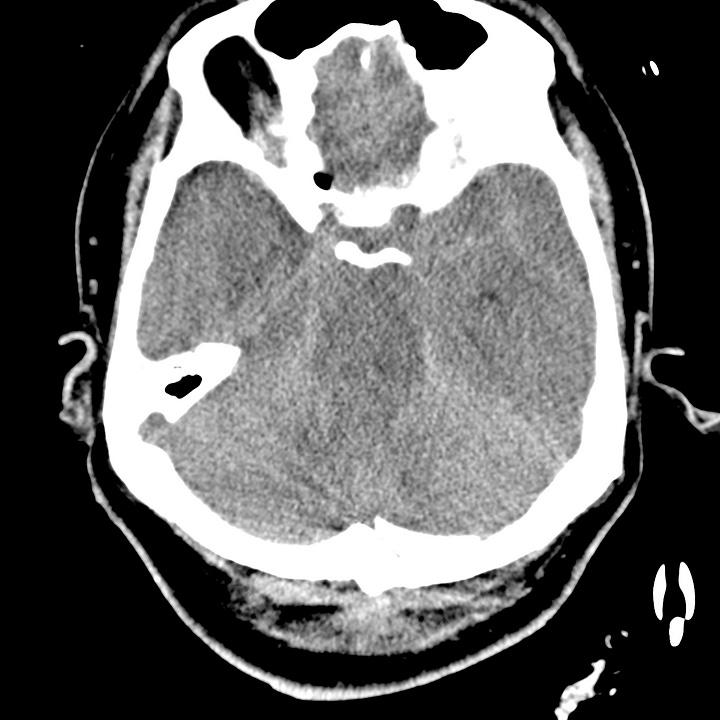
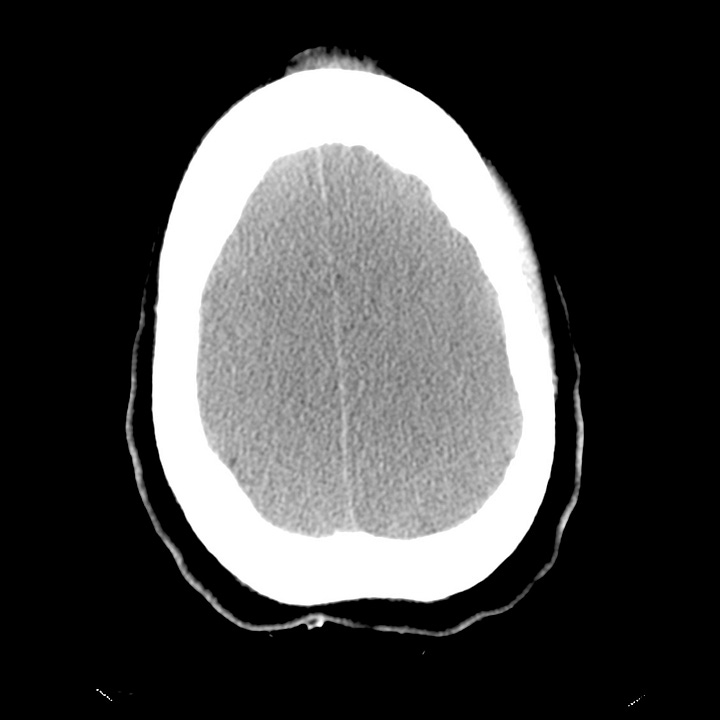
Traumatic cerebral swelling in another patient. Poor gray-white differentiation, sulcal and perimesencephalic cisternal effacement, right frontal subacute subdural hematoma/hygroma, and traumatic convexity subarachnoid hemorrhage.
Hypoxic-anoxic injury results from severe oxygen deprivation and can be seen in cardiac arrest, respiratory failure, and hypotension. While metabolically active gray matter (cortex, basal ganglia, thalami) is preferentially affected, in severe cases, hypoxic-anoxic injury appears on CT as generalized cerebral swelling with diffuse loss of gray-white differentiation. The “pseudo subarachnoid hemorrhage” sign results from normally perfused meninges appearing dense against a background of low attenuation cerebral parenchyma. Preserved cerebellar perfusion can result in a “white cerebellum” sign, and low attenuation changes limited to the basal ganglia and thalami can be seen in less severe cases.

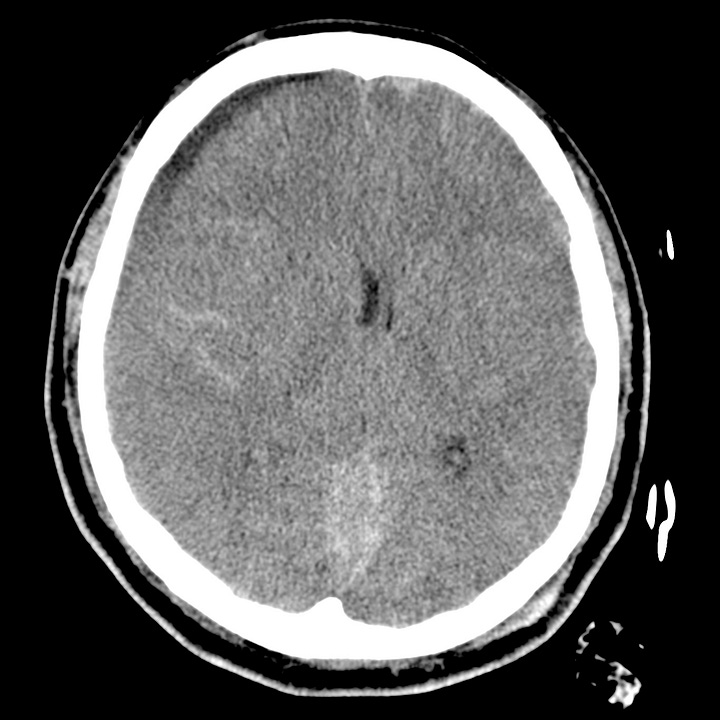
Cerebral swelling due to anoxic injury. Complete loss of gray-white differentiation. Severe ventricular and sulcal effacement.

