Mechanical gastric outlet obstruction results from pyloric or distal gastric malignancy, peptic ulcer disease, gastric polyps, diaphragmatic hernia, caustic ingestion and scarring, pancreatic pseudocysts, and bezoars.

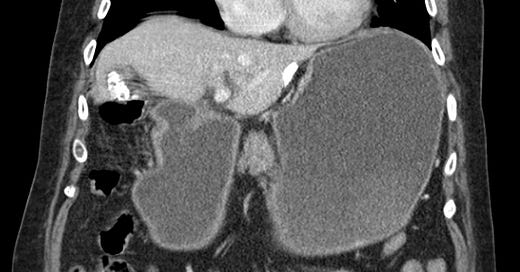
Gastric outlet obstruction due to antral ulcer. The stomach is distended due to pyloric edema associated with a small ulcer. The small bowel and large bowel are collapsed.

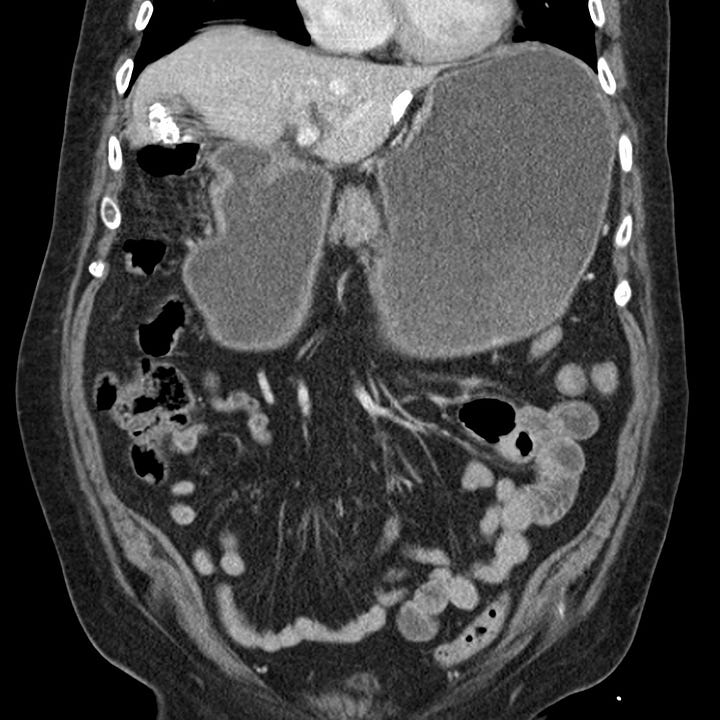
Gastric outlet obstruction due to compulsive hair ingestion. The stomach is obstructed at the pylorus by a heterogeneous intraluminal gastric mass that contains innumerable tiny air pockets (trichobezoar).


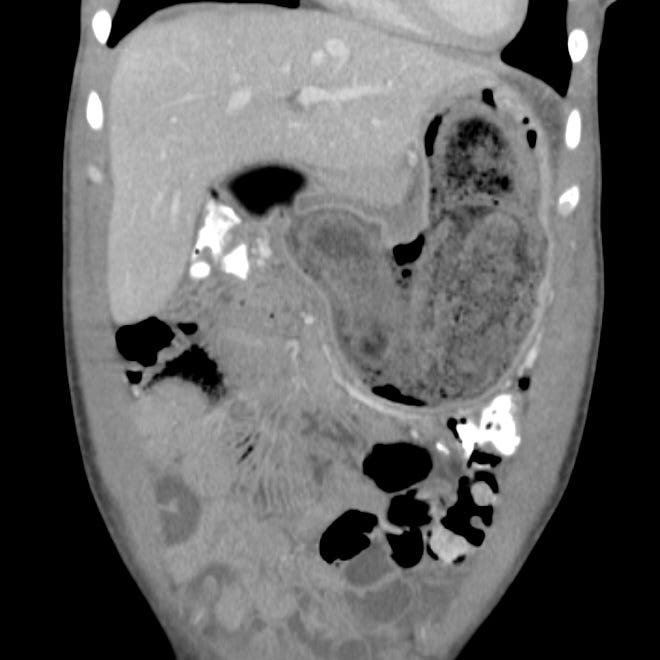
Gastric outlet obstruction due to diaphragmatic hernia. The duodenum and proximal small bowel have herniated through a diaphragmatic defect, resulting in massive gastric dilatation from obstruction just distal to the antrum.
Delayed gastric emptying (gastroparesis) and consequent distention is most often due to diabetes, Parkinson disease, or multiple sclerosis. Gastric and proximal duodenal obstruction can rarely occur in superior mesenteric artery syndrome.
In both extrinsic and intrinsic obstruction, patients present with intermittent vomiting and nausea, which worsen until obstruction is complete. Initially, patients tolerate liquids better than solid food. Progressive obstruction may lead to dehydration, electrolyte abnormalities, and malnutrition. Congenital pyloric stenosis occurs in infants aged 2–6 weeks who present with projectile vomiting after feeding.
Plain abdominal radiographs, upper GI contrast studies with Gastrografin or barium, and CT with oral contrast show gastric dilatation and contrast within an enlarged stomach and can detect gastric neoplasm, ulceration, and adenopathy.