Epidural Hematoma
Brain
Most epidural hematomas (EDH) are of arterial origin and result from calvarial fractures that cross branches of the middle meningeal artery. Hemorrhage under arterial pressure separates the outer layer of the dura from the skull, creating an extraparenchymal intracranial mass that compresses the adjacent brain, leading to ischemia and potential compartmental herniation. Epidural hematomas can enlarge rapidly and, if not treated, are often fatal. With early evacuation, however, the prognosis is good; the skull absorbs most of the energy of impact as it fractures, sparing the under- lying brain parenchyma from direct injury.
An acute arterial EDH is a smooth, hyperdense biconvex extraparenchymal blood collection, limited by the coronal sutures, to which the dura is especially adherent. Hyperacute, active bleeding has an inhomogeneous, swirling appearance due to a mixture of clotted and unclotted blood.
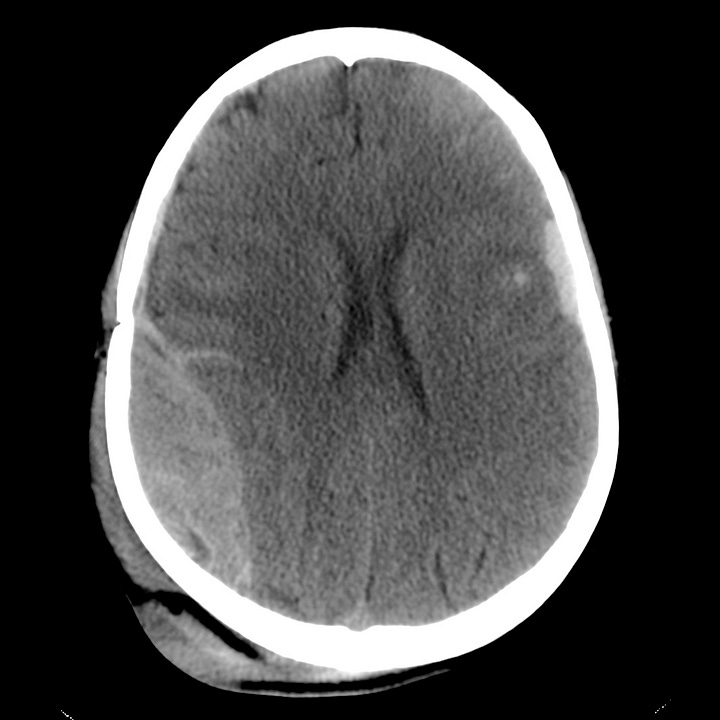
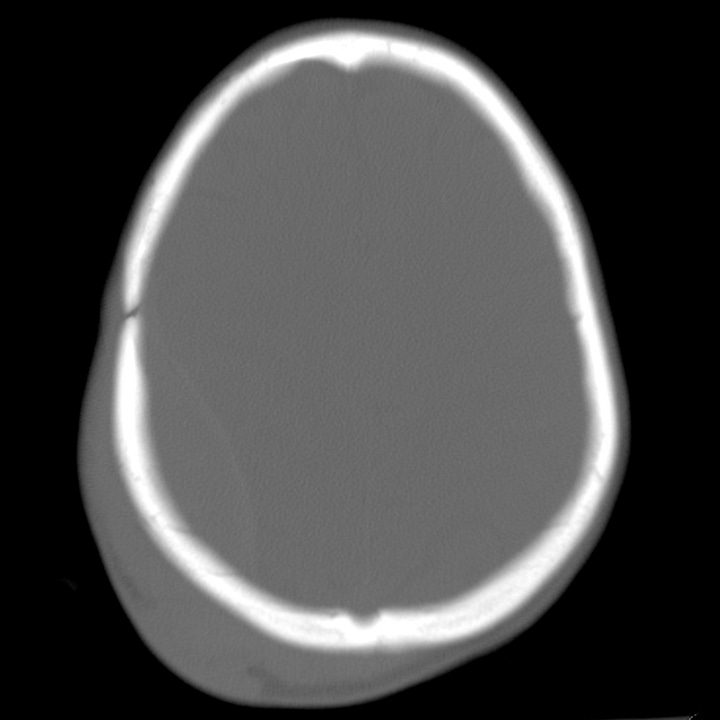
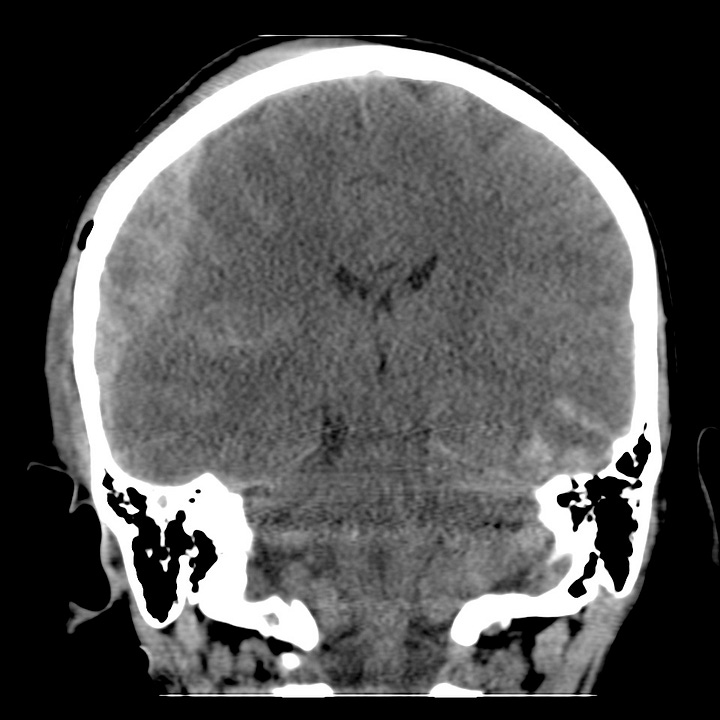

Arterial epidural hematoma. Hyperdense, right parietal, lenticular, extraparenchymal hematoma with maximal thickness 2.7 cm. Ipsilateral cortical sulcal and lateral ventricular compression with minimal subfalcine shift. Contralateral anterior temporal lobe hemorrhagic contusion. Right parietal vertex scalp hematoma and laceration.
Venous epidural hematomas, which account for approximately 10% of EDHs, are the consequence of dural venous sinus disruption or, rarely, diploic vein or arachnoid granulation rupture. They are low-pressure hemorrhages that typically do not enlarge over time and rarely require evacuation. In contrast to arterial hematomas, traumatic venous EDHs often occur in children and are not necessarily associated with skull fractures. They are most commonly seen in the middle cranial fossa adjacent to the greater wing of the sphenoid bone, where venous EDHs are due to disruption of the sphenoparietal venous sinus. They also may follow injury to the sagittal or transverse sinuses and can traverse the tentorium at the occiput or the falx at the vertex.
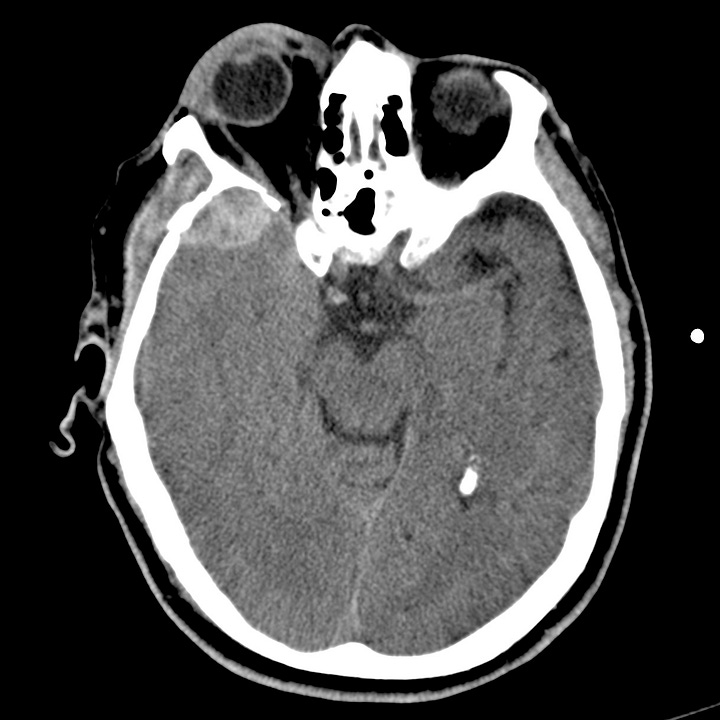
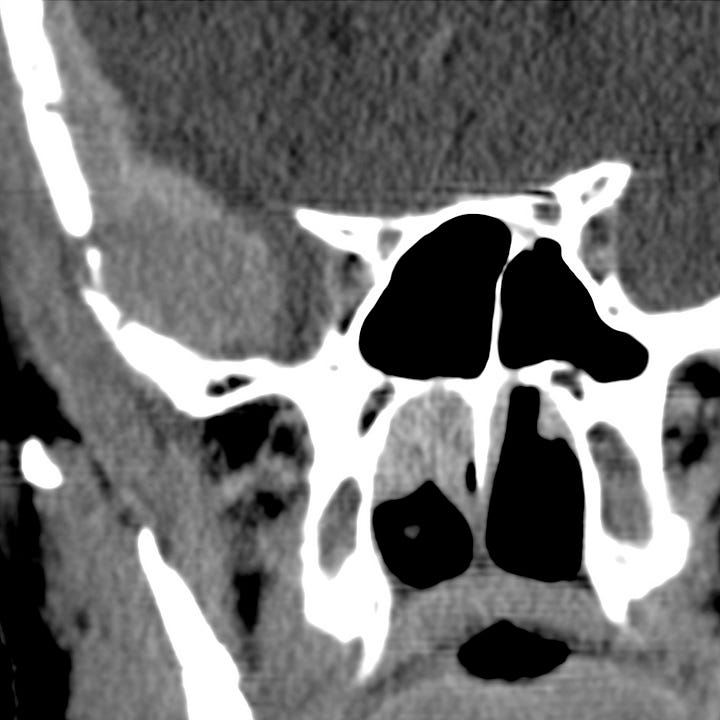
Venous epidural hematoma. Lenticular (1-cm) extraparenchymal mixed-density hemorrhage adjacent to the right sphenotemporal buttress with mild compression of the anterior temporal lobe. Right preseptal periorbital and temporal scalp hematoma. The underlying brain parenchyma is normal, and the perimesencephalic cisterns are patent.

