Duodenal perforation is most often the consequence of underlying peptic ulcer disease, usually due to chronic H. pylori infection or use of non-steroidal anti-inflammatory medications. Perforation can also result from blunt abdominal trauma and can complicate endoscopy and surgery. In the setting of peptic ulcer disease, duodenal perforation is two to three times as common as gastric perforation.
Perforations may be free or contained. In free perforation, intestinal contents spill into the peritoneal cavity, whereas in a contained perforation, leaked fluid is limited by adjacent organs. Free perforation usually presents dramatically with acute pain, abdominal rigidity and tachycardia. Symptoms of contained perforations are usually more subtle and indolent.


Contained perforated duodenum in peptic ulcer disease. Small, contained fluid collection with a focus of air adjacent to the proximal duodenum. On upper gastrointestinal series, contrast extravasates from the narrowed first portion of the duodenum.
Upright or decubitus radiographs show free intraperitoneal air in about two-thirds of patients. When air is visible, it appears as a lucent crescent below the diaphragm on upright chest or abdominal radiograph or as lucency below the antidependent abdominal wall on decubitus views and abdominal CT examinations. On supine radiographs, larger quantities of air may outline the falciform ligament as well as the inner and outer surfaces of the bowel wall (Rigler sign).
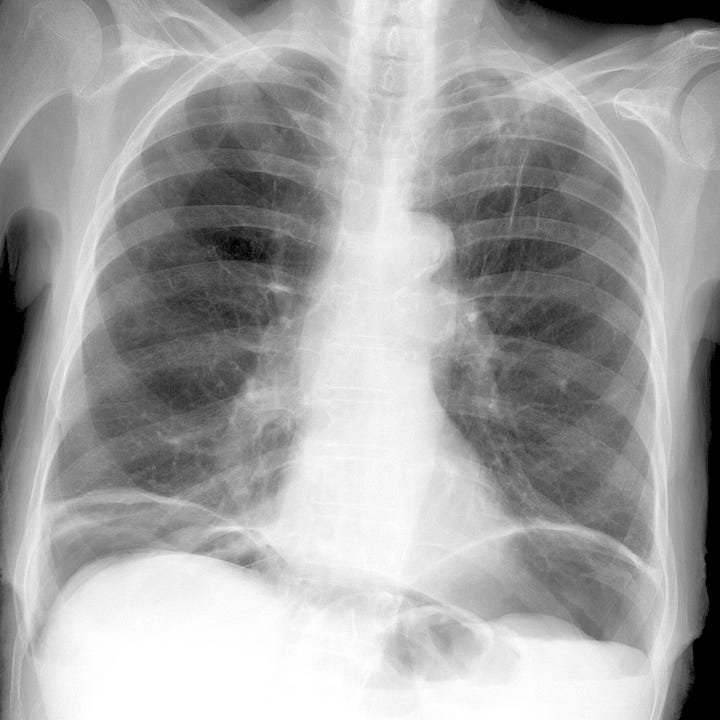

Duodenal perforation with intra-peritoneal air. Extensive free subdiaphragmatic air on upright chest radiograph. Air outlines the inner and outer small-bowel wall on supine abdominal radiograph (Rigler sign).
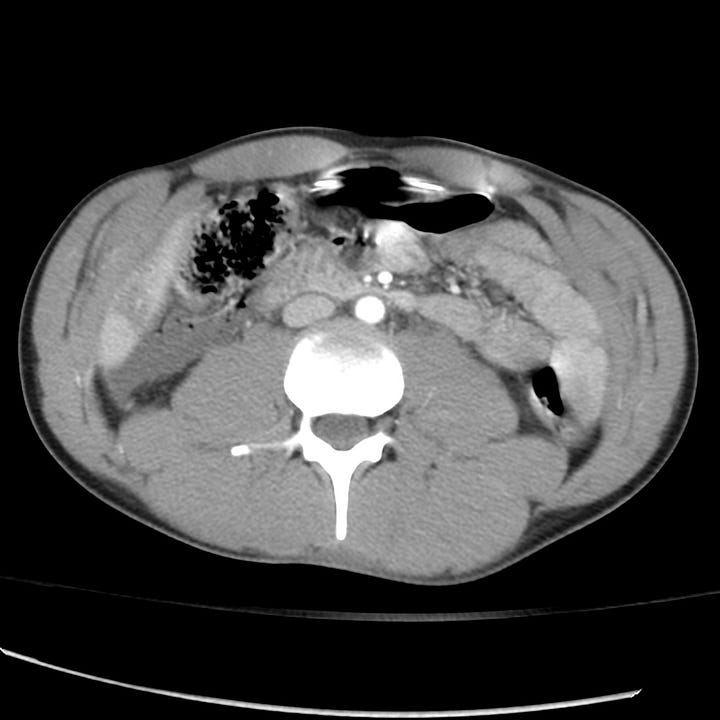

Duodenal rupture in blunt abdominal trauma. Small amount of fluid and several tiny bubbles of air adjacent to the second part of the duodenum. Small inferior hepatic laceration. Free pelvic fluid.
Absent recent surgery or trauma, large amounts of free intraperitoneal air are most often due to a perforated gastric or duodenal ulcer. Smaller amounts can be seen (often only on CT) with perforated diverticulitis or perforated colon carcinoma.
Abdominal CT sensitively identifies free air, intra-abdominal fluid collections, and contrast extravasation; it can often delineate the location and morphology of the perforated viscus. Upper gastrointestinal series can identify ulcers, luminal narrowing, irregularity and extravasation.
Small contained perforations may be treated conservatively. Free perforations typically require either endoscopic or surgical repair.


Worth studying images and text