
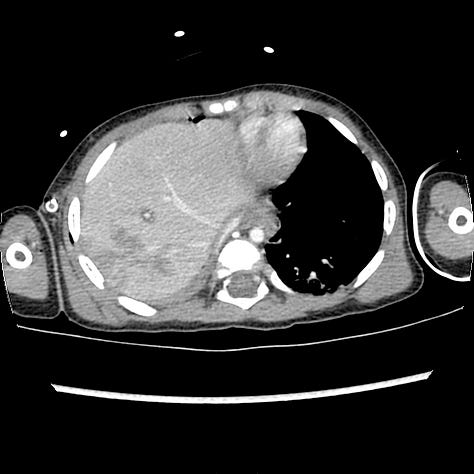
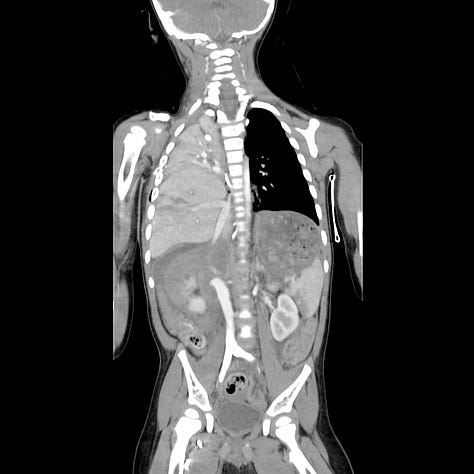
The right hemidiaphragm is elevated and the liver has herniated into the thoracic cavity with leftward tracheal and mediastinal shift. A right hepatic lobe laceration is present.
Blunt impact, with abrupt elevation of intra-abdominal pressure sometimes results in diaphragmatic rupture, more commonly on the left side. Abdominal viscera can herniate through the defect, and result in acute or delayed bowel obstruction, which may occur years after the primary injury. In patients on mechanical ventilation, positive intrathoraci pressure can prevent herniation and make early diagnosis more difficult.
Penetrating trauma to the back or upper abdomen can also result in diaphragm laceration, but the defect is usually smaller than tears resulting from blunt trauma.
In both cases, the integrity of the diaphragm should be carefully assessed, particularly in the ventiated patient and in any patient with penetrating trauma that may traverse the diaphragm. Remote laceration is a consideration in any patient with acute bowel obstruction and a past history of torso trauma.
CT is the optimal imaging technique, although plain radiographs and ultrasound may also be diagnostic. Direct imaging signs include diaphragmatic discontinuity, waistlike constriction of herniated viscus (collar sign), and the dependent viscera sign, in which abdominal viscera appear to contact the posterior thoracic wall. Indirect findings include hemidiaphragm elevation > 4 cm, a nasogastic tube that does not descend below the expected position of the gastroesophageal junction, diaphragmatic thickening, injury on both sides of the diaphragm, or hemothorax without obvious thoracic injury.
Penetrating injuries are less likely than blunt injuries to result in organ herniation, as the diaphragmatic defect is typically smaller (1 cm for penetrating injury compared with 5–6 cm in blunt trauma)
