Stretching, twisting, or compression of the neck can result in carotid or vertebral artery dissection, which is characterized by intimal injury, intramural hemorrhage, vascular narrowing, and potential intravascular thrombosis with embolization. When the subendothelium is exposed to blood, it induces a coagulation/repair process that can form small clots. These can embolize to the cerebral circulation and lead to an acute arterial distribution infarct. Dissection is an important cause of stroke in patients under 45 years and should be considered in the young or middle-aged adult with new-onset neurologic deficits.
Dissection may follow major blunt neck trauma or trivial injury, including head turning or chiropractic manipulation. Many patients have no history of prior neck trauma. Connective tissue disorders such as Marfan and Ehlers-Danlos syndromes may predispose to spontaneous or minimal-injury dissection. In high-velocity trauma, carotid injury often occurs at the junction of the cervical and petrous segments of the internal carotid artery, where the vessel enters the skull. Patients without a history of acute trauma may present with unilateral headache, retro-orbital pain, facial pain, or upper neck pain. Ipsilateral Horner syndrome without anhidrosis or retinal ischemia are more specific findings that should prompt urgent imaging investigation. If a cerebral infarct has already occurred, hemiparesis, hemisensory loss, or aphasia may be the dominant finding.
CT without contrast is the initial study obtained in head trauma and suspected acute cerebral infarct, but it is not sensitive for detection of vascular injury. CT angiography (CTA) is the study of choice for detecting either dissection or pseudoaneurysm. Clinical indications for CTA include: Glasgow coma scale score < 6, diffuse axonal injury, severe facial fractures, skull base fractures, upper cervical spine fractures, fractures involving the transverse vertebral foramina, neck hematoma, and hanging mechanisms.
CTA accurately evaluates most acute cervical vascular injuries. Conventional angiography is reserved for cases in which endovascular therapy such as embolization, angioplasty, and stent placement is contemplated. In carotid artery dissection, CTA shows an eccentric, narrowed, arterial lumen associated with a thick vascular wall, often greater in diameter than that of the contralateral artery. MRI is sensitive for arterial dissection and is often obtained in the patient without a history of significant trauma. On cross-sectional T1-weighted images (optimally with fat suppression), the intramural hematoma appears as an isointense or hyperintense crescent in the vessel wall. After several days, the hematoma becomes hyperintense on T1 MRI.
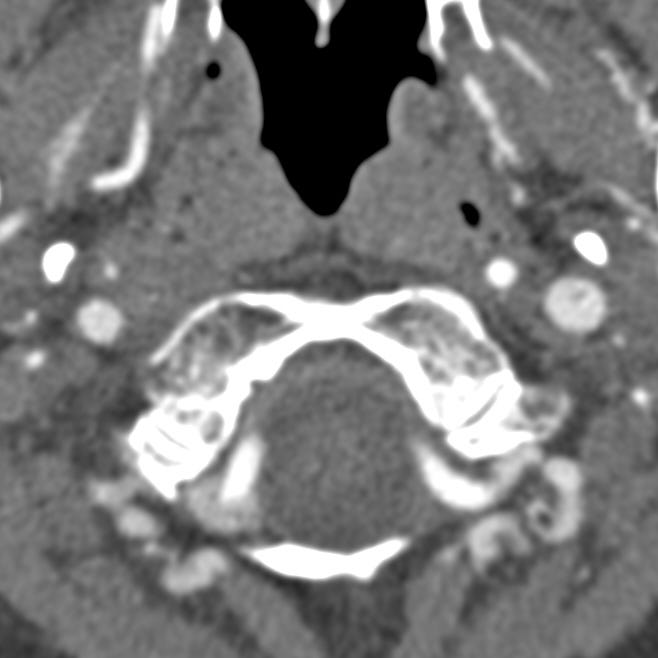
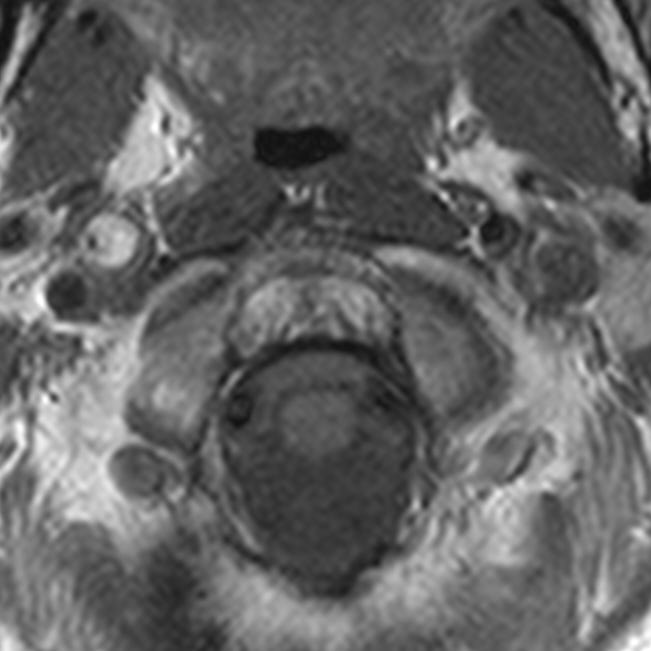
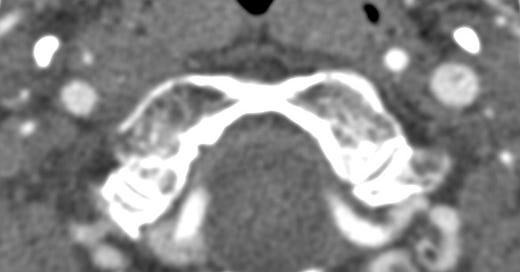
Carotid dissection. CTA shows marked narrowing of the right internal carotid artery (medial to the styloid process and anterior to the jugular vein). The left carotid artery is normal. T1-weighted MRI shows a large, high-signal intramural hematoma with severely narrowed luminal flow void.


Bilateral traumatic carotid injury. Generalized cerebral swelling with absent gray-white differentiation. Normal opacification of the posterior cerebral arteries with complete absence of cavernous carotid artery opacification. Occluded right and left internal carotid arteries ~ 1-2 cm proximal to the skull base (coronal images). Left petrous carotid contrast is due to retrograde filling from vertebral circulation/posterior communicating arteries.
Carotid pseudoaneurysm is an uncommon complication of neck trauma, especially penetrating injury. Blood that extravasates from a vascular tear accumulates in and is contained by the adjacent tissues, forming a contained outpouching that has the potential for expansion and later catastrophic rupture.
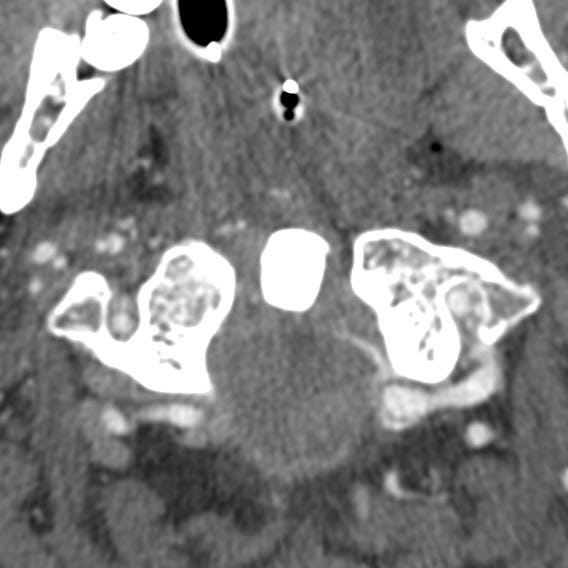

Carotid pseudoaneurysm following choking injury. A 1 mm pseudoaneurysm arises from the cervical portion of the right internal carotid artery.