The primary supporting ligaments of the cervical spine are the anterior longitudinal ligament, the posterior longitudinal ligament, and the posterior ligamentous complex.
Cervical spine ligamentous anatomy. (Illustration courtesy of Mark Bernstein, MD)
Abrupt extension followed by hyperflexion, or hyperflexion with axial impact (typically head-on motor vehicle collisions and diving accidents) results in injury to these structures that begins posteriorly and progresses anteriorly with increasing energy transfer. Imaging findings include: interspinous widening, uncovered facets, widened posterior disc space, focal kyphosis, and anterior subluxation.
The spectrum of hyperflexion injuries, in order of severity/instability includes: Hyperflexion sprain, in which only the posterior ligamentous complex (PLC) is disrupted, anterior subluxation, in which both the PLC and posterior longitudinal ligament (PLL) are torn, and bilateral facet dislocation, in which all three supporting ligaments are torn. Severe injuries may be associated with avulsion of the anterior inferior vertebral body and are referred to as hyperflexion teardrop fractures.
A hyperflexion sprain is stable, but any degree of anterior vertebral subluxation, facet subluxation, or facet dislocation indicates an unstable injury. MRI and/or delayed flexion and extension radiographs (after muscle spasm related to the acute injury has resolved) can be used to better assess ligamentous injury and stability.
Hyperflexion sprain. Slight kyphotic angulation at C5–C6 with subtle splaying of the spinous processes indicates a posterior ligamentous complex injury.
The clay shoveler fracture is a horizontal fracture of a lower cervical spinous process originally described in workers who would abruptly contract their cervical muscles and flex the neck while shoveling heavy clay. The fracture may also result from direct impact and other complex mechanisms. Clay shoveler fractures are stable, as they do not involve the vertebral ring and are often incidentally discovered years after a forgotten injury.
Clay shoveler fracture. Acute, transverse oblique, minimally displaced fractures limited to the spinous processes of C5 and C6.
In bilateral interfacet dislocation, the ALL, PLL and PLC are all disrupted. This injury is uncommon, extremely unstable, and associated with a high risk of spinal cord damage. On lateral cervical spine radiograph or sagittal CT reformation, the inferior articulating facet of the upper vertebra is displaced and locked anterior to the superior articulating facet of the lower vertebra. The upper vertebral body may be anteriorly displaced by up to 50% relative to the lower one. Disk space widening, interspinous widening as well as small facet fractures may be seen.

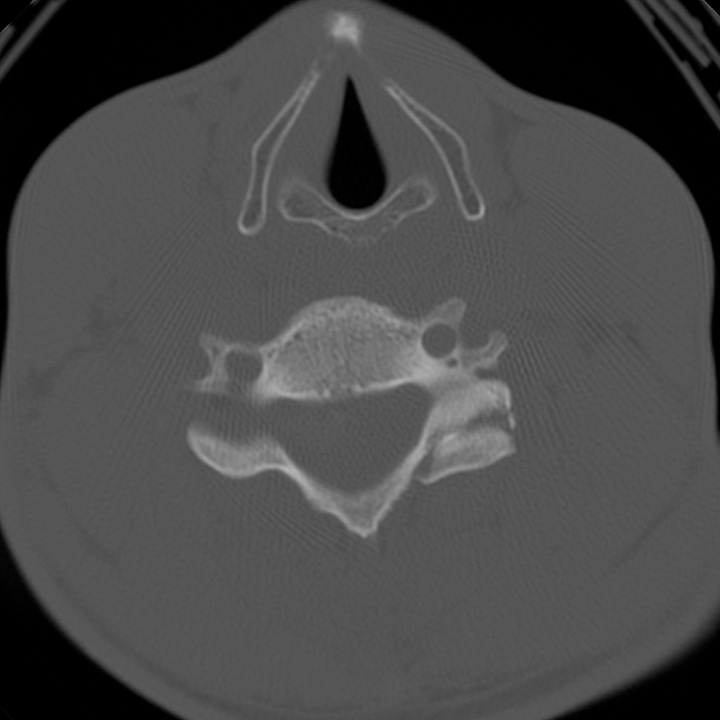


Bilateral interfacet dislocation. Focal kyphosis and anterolisthesis of C5 with respect to C6. The right inferior articulating facet of C5 is “perched” on the superior articulating facet of C6, resulting in an un- paired “naked” facet on the axial image. The left inferior articulating facet of C5, which should lie posterior to the C6 superior articulating facet, is dislocated anteriorly, resulting in the “reverse hamburger sign,” in which the dorsal surface of the C5 facet contacts the anterior surface of the C6 facet. Small bilateral facet fractures are present.
Unilateral interfacet dislocation is a variant in which forced neck flexion is associated with simultaneous rotation, resulting in dislocation of only one facet. The diagnosis may be delayed, as patients often have either no neurologic deficit or isolated radiculopathy, and CT findings may be subtle. Because dislocation occurs at the moment of injury, and can spontaneously reduce prior to imaging, a mildly widened facet joint may be the only clue to diagnosis.
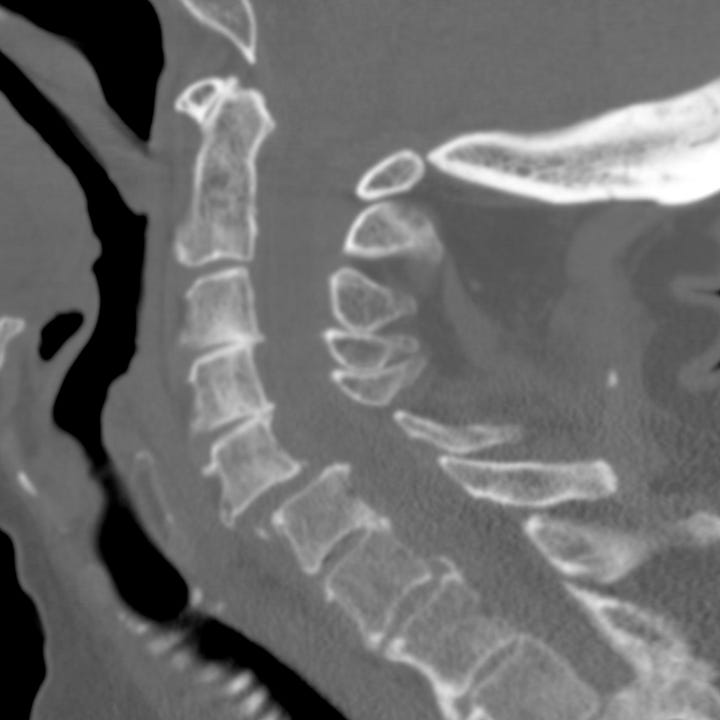

Unilateral interfacet dislocation progressing to bilateral interfacet dislocation. Sagittal reformations show initial study with ~ 25% anterolisthesis of C5 with respect to C6; axial images (not shown) confirmed UID. Subsequent CT obtained after acute development of paraparesis show ~ 75% anterolisthesis and BID. Although UID is often considered relatively stable, it may be seen transiently in the presence of severe ligamentous disruption characteristic of BID.
Hyperflexion teardrop fractures are the most devastating of the hyperflexion injuries and are due to severe axial loads with anterior and posterior ligamentous disruption, fracture of one or more vertebrae, and at least transient subluxation or vertebral body retropulsion. Anterior spinal cord injury is virtually always present, and patients suffer acute quadriplegia with loss of pain and temperature sensation but with variable preservation of the dorsal tracts that provide vibratory sense and proprioception.
CT with sagittal reformations shows a triangular fragment avulsed from the anterior inferior corner of a mid or lower vertebral body as well as focal kyphosis and posterior element distraction. The avulsed fragment frequently remains aligned with the anterior margins of the adjacent vertebrae, while the posterior fragment is displaced into the spinal canal. A typical burst fracture occurs when the injuring force is primarily axial; sagittal split, loss of vertebral height, dorsal fragment retropulsion, and laminar fracture are hallmarks.

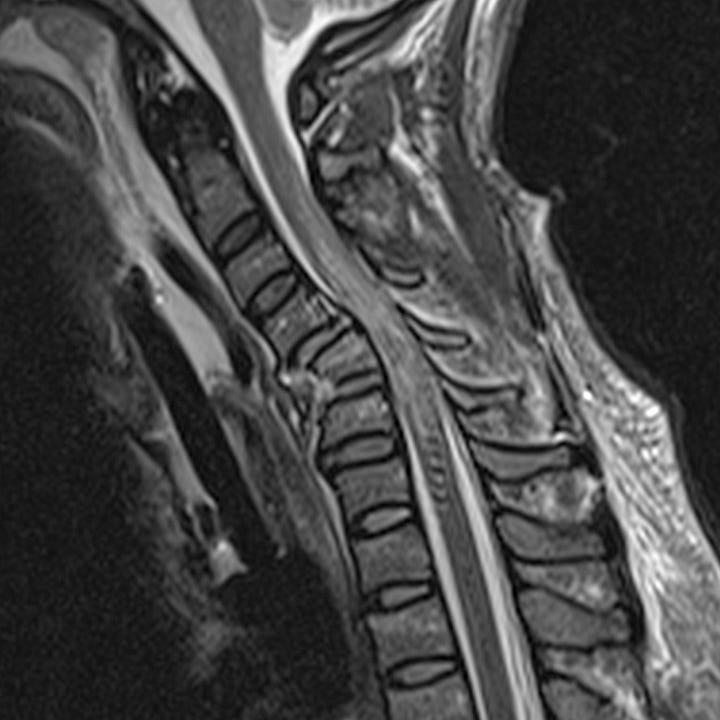

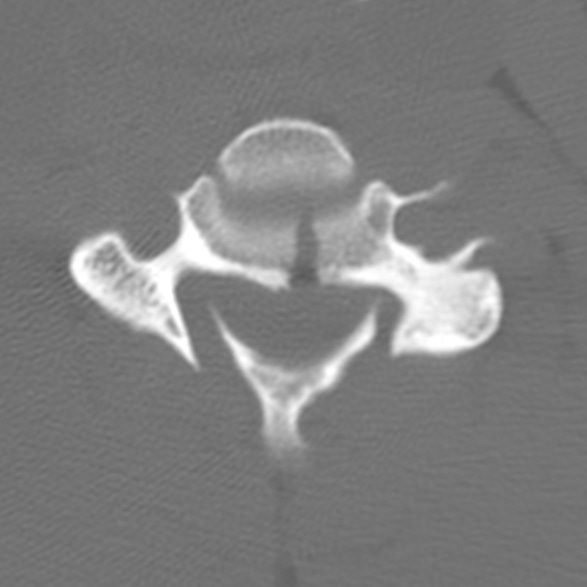
Hyperflexion teardrop fracture. Small anterior triangular fragment with posterior displacement of the C5 vertebral body and focal kyphotic angulation. T2-weighted sagittal MRI shows anterior prevertebral and nuchal ligament edema, fracture and marrow edema in C5, and spinal cord edema extending from C3 to C6. Coronal and axial images show typical sagittal split, which may be inapparent on lateral radiographs or sagittal reformations.
Operative spinal fusion is necessary for hyperflexion teardrop fractures, burst fractures, and both types of interfacet dislocation in order to restore mechanical stability. Hyperflexion sprains and clay shoveler fractures can often be treated conservatively.




