Multipart fractures of the C1 ring with fragments displaced away from the C2 odontoid result from axial loading forces transmitted throught the occipital condyles. One common mechanism is diving headfirst into shallow water. Because the fracture widens rather than narrows the spinal canal, patients present with pain but without neurologic dysfunction. Associated spinal cord injury is usually absent unless there is a retropulsed fragment. Fracture stability depends primarily on whether or not the transverse atlantal ligament is intact.
The “classical” Jefferson fracture is a four-part fracture with bilateral anterior and posterior arch fractures.



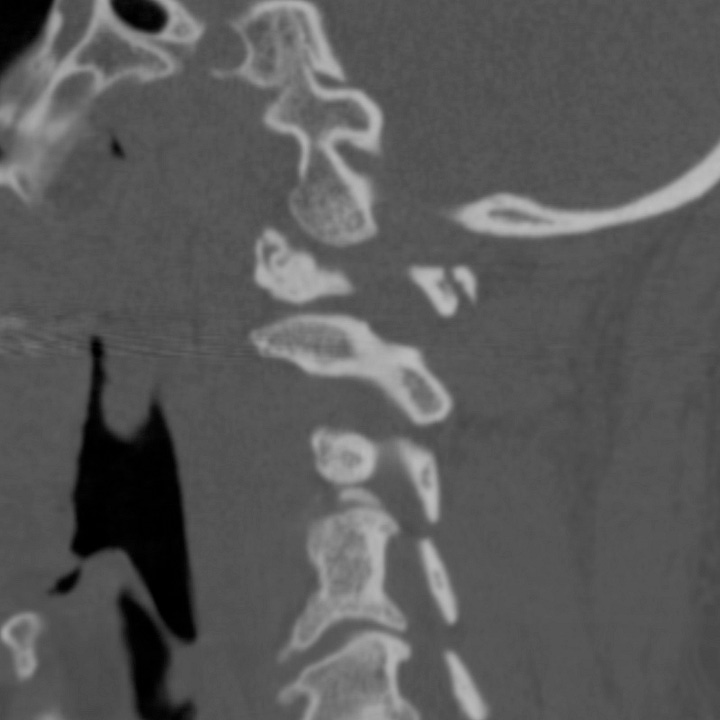
“Classical” Jefferson fracture. Unstable, four-part fracture involving the anterior and posterior arches of C1 with combined transverse atlantodental intervals of 15 mm and slight lateral displacement of the C1 lateral mass with respect to the body of C2.
Two- and three-part fractures indicate eccentric loading and usually involve one lateral mass and the adjacent occipital condyle.

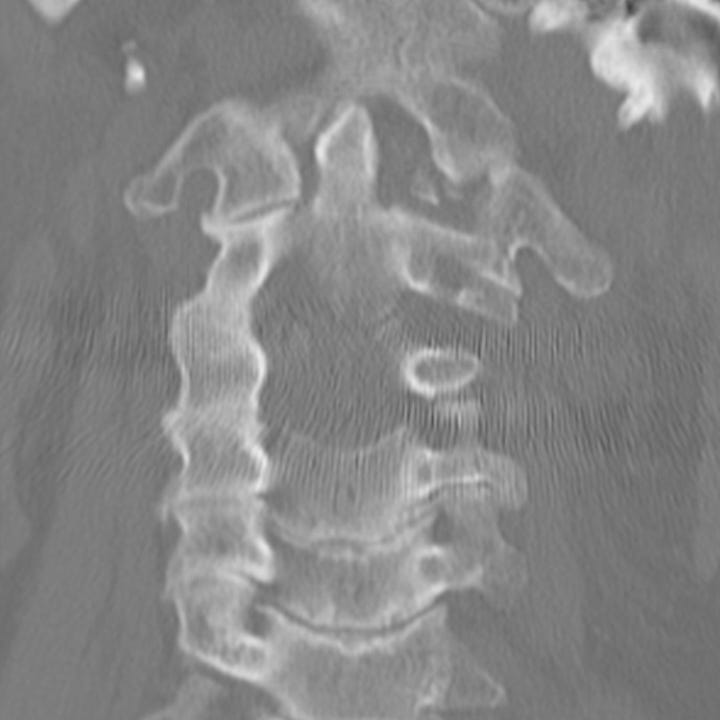
Lateral mass C1 fracture (“atypical” Jefferson fracture). Comminuted C1 left lateral mass fracture with three major fragments. The dens is normally related to the anterior arch of C1 indicating integrity of the atlantodental ligaments.
On coronal reformations the C1 lateral masses are displaced away from the odontoid. If the combined lateral atlantodental intervals are > 7 mm, transverse ligament rupture is possible. Sagittal reformations show prevertebral soft tissue swelling as well as a widened atlantodental interval. The normal atlanto-dental interval is ≤ 3 mm in adults and ≤ 5 mm in children. An atlantodental interval > 6 mm indicates definite transverse ligament disruption.
Multidetector CT best delineates the C1 ring fractures, their extent of displacement, and any other synchronous fractures of the cervical spine. Minimally displaced fractures may be treated conservatively with hard collar immobilization. If the transverse atlantal ligament is disrupted, the injury will likely require halo placement or C1–C2 surgical fixation




Why isn't it called the Adams fracture?