Boerhaave syndrome refers to acute esophageal rupture following an episode of retching or vomiting. It is the consequence of a sudden increase in intraluminal esophageal pressure against the closed cricopharyngeus muscle, with tearing at the weakest part of the esophagus, the posterior esophageal wall near the esophageal hiatus. Boerhaave syndrome comprises ~ 15% of esophageal perforations (most others are complications of surgery or endoscopy).
Alcoholism and acute over-eating are risk factors. The typical patient is a man between the ages of 50 and 70 with chest pain and subcutaneous emphysema following an episode of forceful retching or vomiting. Dyspnea, blood-stained vomitus, and, in severe cases, hypovolemic shock may be present.
Consequences include hydropneumothorax, mediastinitis, empyema, pericarditis, sepsis and shock. Overall mortality is ~ 30%. A delay in diagnosis and treatment increases mortality significantly; 50% after 24 hours, and 90% after 48 hours. Treatment consists of early surgical repair and drainage.
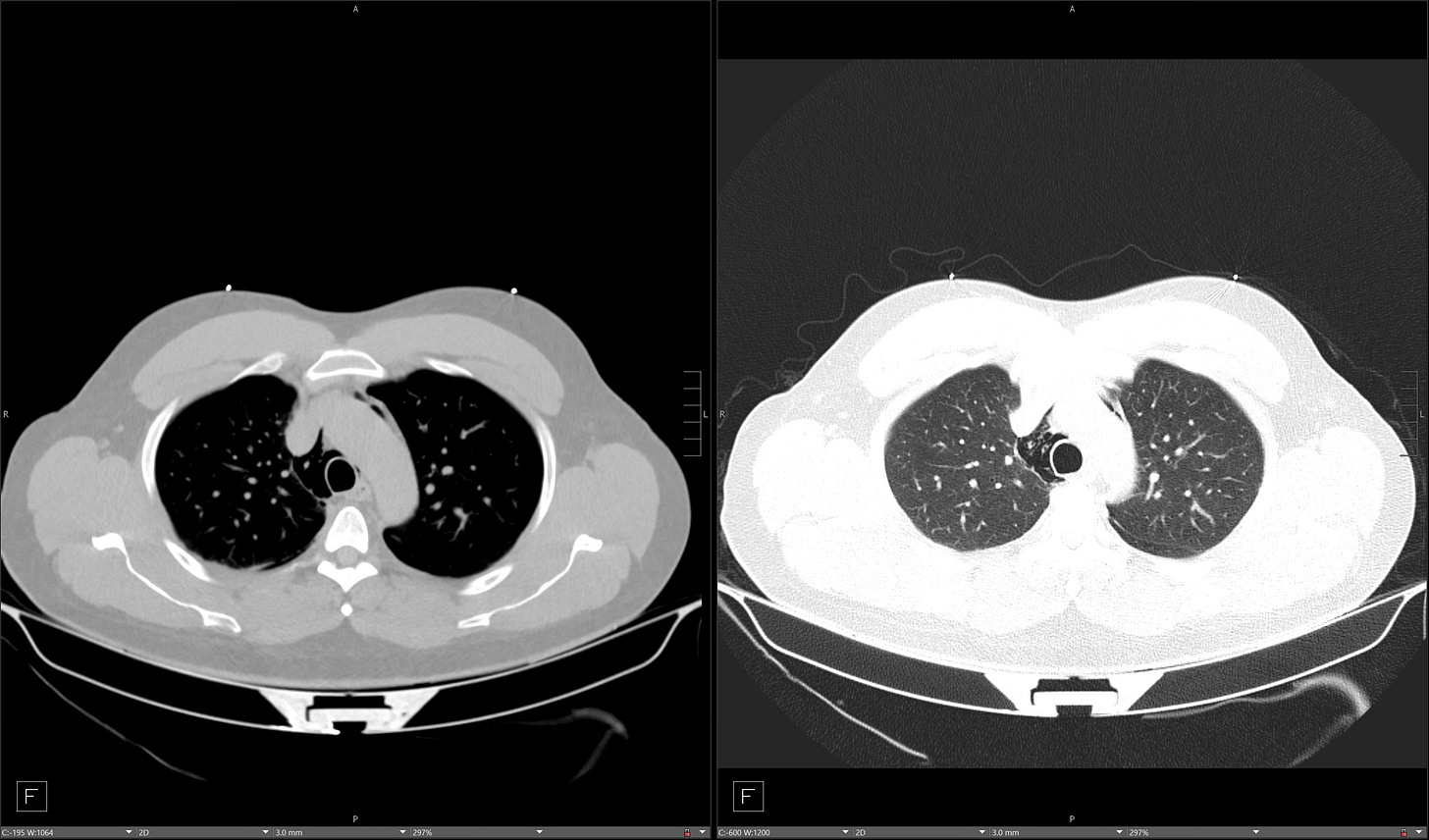
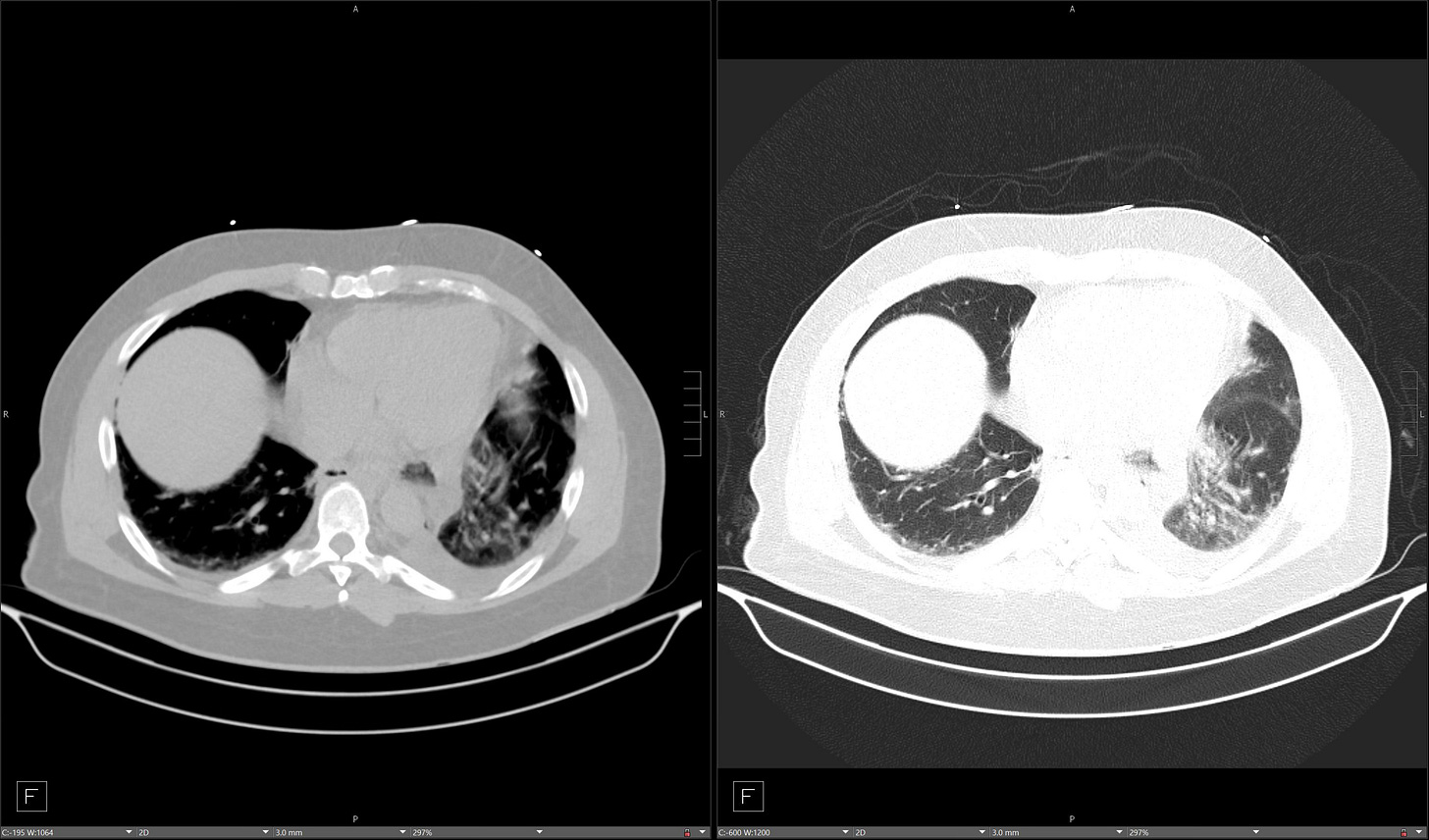
Pneumomediastinum, sometimes with cervical subcutaneous emphysema, and left pleural effusion are the radiographic hallmarks of Boerhaave syndrome. CT shows focal distal esophageal wall thickening, mediastinal fluid, pneumomediastinum, and pleural effusion. Esophagogram with water-soluble contrast material is diagnostic and demonstrates contrast extravasation into the mediastinum and/or pleural space just proximal to the esophageal hiatus.
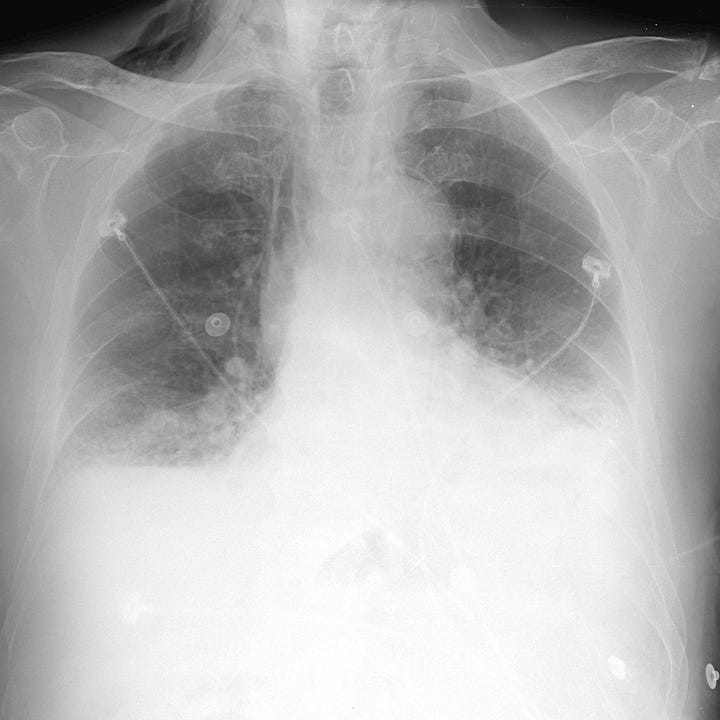

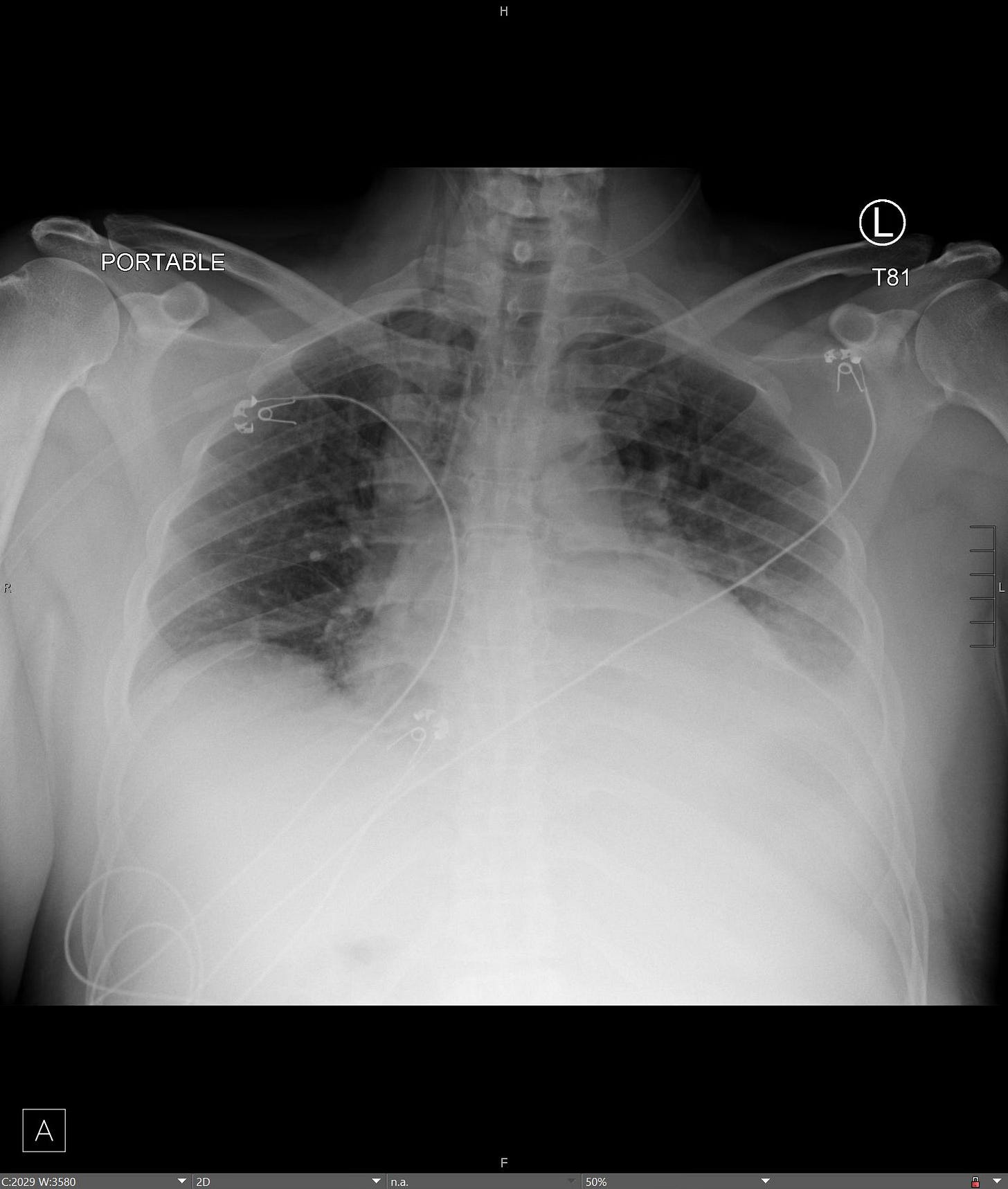
Esophageal rupture after vomiting. Subcutaneous emphysema, pneumomediastinum, and left pleural effusion. Gastrografin esophagogram shows extensive extravasation of contrast into the mediastinum and pleural space.
Esophageal rupture after vomiting. Radiograph and CT show pneumomediastinum, lower cervical soft tissue emphysema, and left pleural effusion. Esophagram demonstrates distal esophageal defect and extravasation of contrast.