Achalasia is a disorder of esophageal motility that results from failure of coordinated peristalsis and relaxation of the lower esophageal sphincter with swallowing. Degeneration of the myenteric neural plexus, which regulates peristalsis, leads to increased lower esophageal pressure and dilatation. Patients present with progressive dysphagia, vomiting, malodorous breath, aspiration, and weight loss. Complications of long-standing achalasia include esophageal carcinoma, aspiration pneumonia, esophagitis, and airway obstruction. Most cases are idiopathic, but achalasia can be a consequence of chronic Chagas disease (American Trypanosomasis), a parasitic infection endemic to Central and South America that can result in achalasia, cardiomyopathy and colonic dilatation.
Barium esophagram shows a dilated distal esophagus, aperistalsis, and absent lower esophageal sphincter relaxation, evidenced by a “bird’s beak” appearance to the stenotic gastroesophageal junction. Plain chest radiographs are rarely diagnostic, but the food-filled distended esophagus or a mediastinal air-fluid level may be seen. The gastric air bubble may be small or absent. Esophagoscopy with manometry can be performed to document increased sphincter pressure and exclude complicating esophagitis or neoplasm.
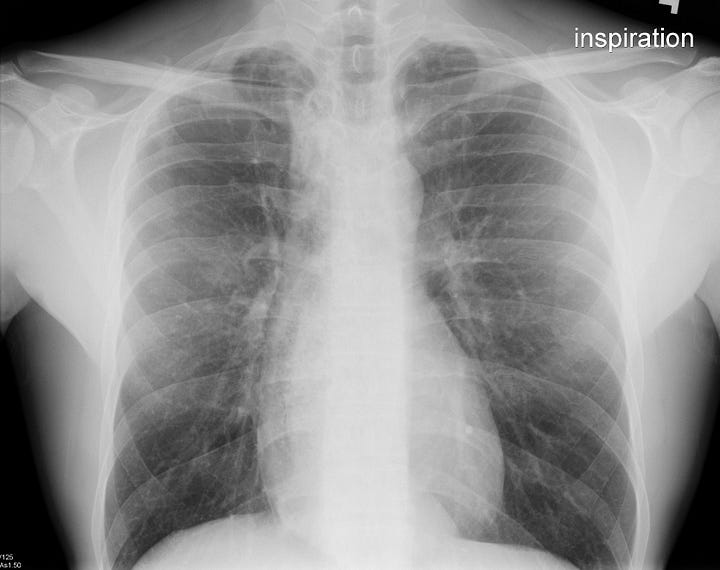

Achalasia. The mediastinum is widened, with a double cardiac shadow along the right heart border. The esophagus is expanded and filled with granular material corresponding to retained food/fluid.


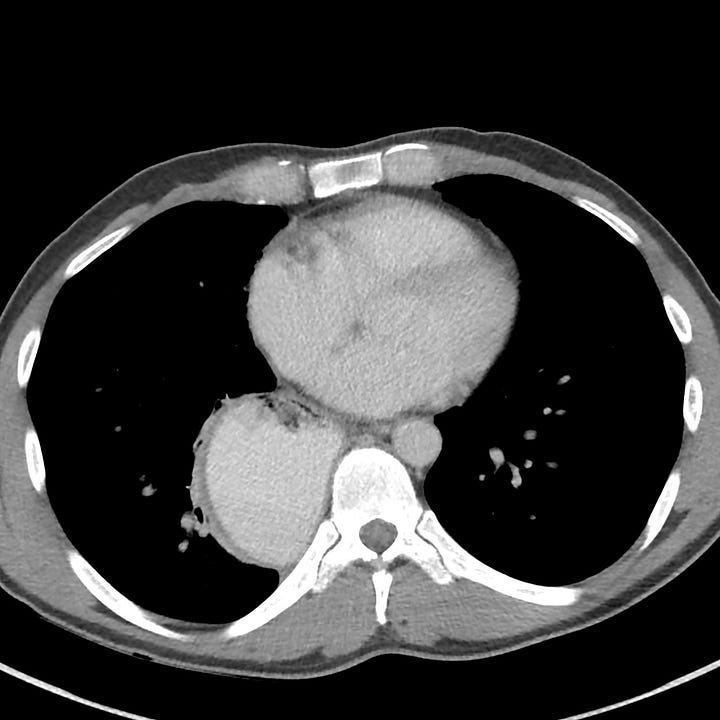
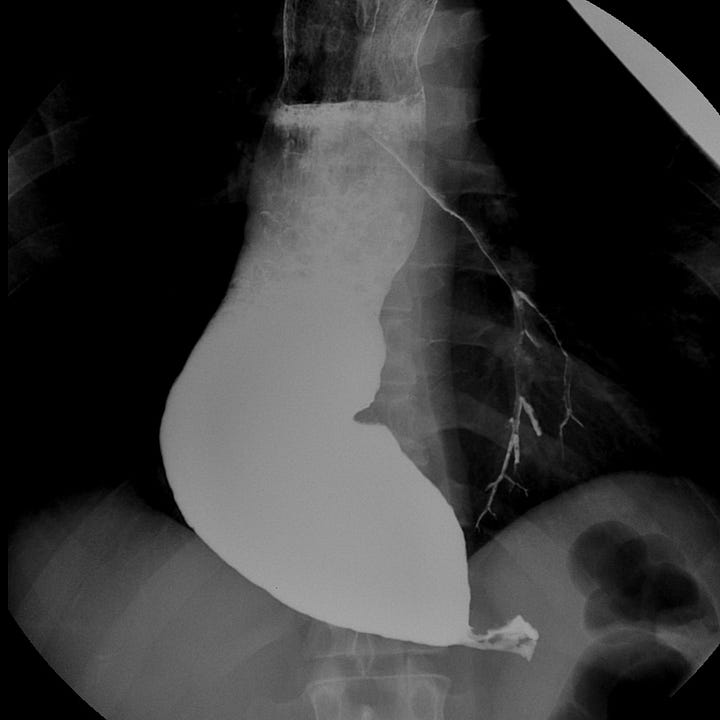
Achalasia. Double cardiac shadow along the lower right heart border on frontal radiograph with retrocardiac density on lateral view. CT and esophagram show gross esophageal dilatation proximal to stenosis (“bird beak”) at the gastroesophageal junction. Incidental barium aspiration.
Treatment aims to reduce lower esophageal sphincter pressure by surgical myotomy, dilation, or endoscopic injection of botulinum toxin.



